LEWIS KATZ SCHOOL OF MEDICINE AT TEMPLE UNIVERSITY | TEMPLE UNIVERSITY HEALTH SYSTEM
SUMMER 2019
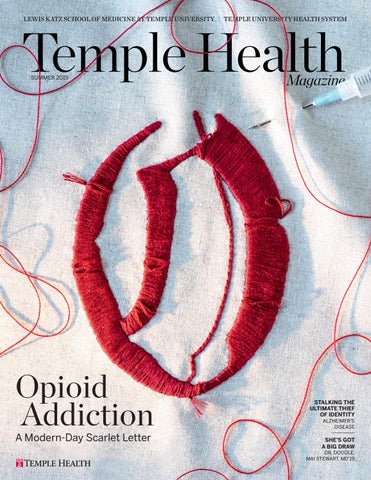
Opioid Addiction A Modern-Day Scarlet Letter
STALKING THE ULTIMATE THIEF OF IDENTITY ALZHEIMER’S DISEASE
SHE’S GOT A BIG DRAW DR. DOODLE, MAI STEWART, MD’19
AGENDA
Temple Health Magazine
EDITOR
Giselle Zayon
Temple Health giselle.zayon@tuhs.temple.edu DESIGN & ART DIRECTION
Magazine
B&G Design Studios
Temple Health Karen Brooks WRITERS & CONTRIBUTORS
Magazine
JoAnne DeSanto-Bonewicz Christopher Guadagnino Meredith Mann Jennifer Reardon Andrew Smith Jeremy Walter BUSINESS MANAGER
Younndia Rush ADMINISTRATION
Christopher Guadagnino, PhD
Mystery and Mastery
OPPOSITE PAGE: JOSEPH V. LABOLITO; KAISER: COURTESY KAISER
A
Director, Communications
Jessica Lista Director, Alumni Relations
bsent human connection, medicine is little more than a transaction, I told the Class of 2019 at the Lewis Katz School of Medicine Commencement on May 10. So work to standards of academic excellence, but remember that half the cure is the care, I advised. The root of the word “doctor” comes from the Latin: Docere, to teach, to serve. One of the oldest forms of service leadership, doctoring is the exercise of power in service to others. It makes the improvement of other people’s lives the currency of your personal gain. Whatever changes unfold in the health care system in this country, medicine must remain a united community of healers, a safe house in every storm. Preserve the sacred doctor-patient bond. Mastery is something to strive for in medicine, with the recognition that it can never be entirely achieved. Subject to new discoveries, our best practices, protocols, and paradigms will continue to evolve. So use your knowledge judiciously and confidently, yet make your commitment to learning lifelong, I said to the graduates. Remember, just one letter separates mastery from mystery. So as you go out into the world, do what you learned to do at Temple: Devote yourself, heart and mind, to advancing that ever-unfolding edge.
CONTACT US
Office of Communications 3509 N. Broad Street Philadelphia, PA 19140 215-707-4839
TempleHealth.org 1-800-TEMPLEMED Lewis Katz School of Medicine Temple University Hospital Temple University Hospital Episcopal Campus Temple University Hospital Northeastern Campus Fox Chase Cancer Center Fox Chase Cancer Center at Buckingham Fox Chase Cancer Center Medical Group Jeanes Hospital Temple Health Oaks Temple Health Center City Temple Health Elkins Park Temple Health Ft. Washington Temple ReadyCare Temple Physicians, Inc. Temple Faculty Practice Plan Temple Transport Team
Larry R. Kaiser, MD, FACS
Senior Executive Vice President for Health Affairs, Temple University The Lewis Katz Dean at the School of Medicine Professor of Thoracic Medicine & Surgery, Lewis Katz School of Medicine President & CEO, Temple University Health System
Temple Health refers to the health, education, and research activities carried out by the affiliates of Temple University Health System, Inc. (TUHS), and the Lewis Katz School of Medicine at Temple University. TUHS neither provides nor controls the provision of health care. All health care is provided by its member organizations or independent health care providers affiliated with TUHS member organizations. Each TUHS member organization is owned and operated pursuant to its governing documents. It is the policy of Temple Health that there shall be no exclusion from, or participation in, and no one denied the benefits of, the delivery of quality medical care on the basis of race, ethnicity, religion, sexual orientation, gender, gender identity/ expression, disability, age, ancestry, color, national origin, physical ability, level of education, or source of payment.
SUMMER 2019 | TEMPLE HEALTH MAGAZINE |
1
30
SUMMER 2019
CONTENTS
FEATURES
10 Opioid Addiction A Modern-Day Scarlet Letter BY GISELLE ZAYON
16 Identity Theft
Chasing Down Alzheimer’s Disease BY GISELLE ZAYON
22 Dr. Doodle Mai Stewart, MD ’19 BY MICHAEL VITEZ
DEPARTMENTS
26 Inside Story The Writing of Students & Staff
30 Quest Ellen Unterwald, PhD The Biology of Addiction
32 Change Agent
LEFT: CARDONI; TOP RIGHT: MAI STEWART, MD; BOTTOM LEFT: CLINT BLOWERS; BOTTOM RIGHT: ANN CUTTING
Michael A. Young, MHA, FACHE CEO, Temple University Hospital
34 Tools of the Trade The Hemolung Respiratory Assist System
36 Timeline Department of Anatomy & Cell Biology
22
44 So Noted Quotes & Quips
45 Artful Ending The Kappa Opioid Receptor IN EVERY ISSUE
1 Agenda
BY LARRY KAISER, MD, FACS
4 Currents News Roundup
40 Impact Alumni Leaders & Philanthropists ON THE COVER: Illustration by Meghan Willis; photography
by Ann Cutting.
4
16 SUMMER 2019 | TEMPLE HEALTH MAGAZINE |
3
CURRENTS EDUCATION & ENGAGEMENT
RESEARCH & CLINICAL CURRENTS
APPOINTMENTS & ACCOLADES
Low-Salt Solutions
N
early 40 percent of adults in Philadelphia have high blood pressure. And dietary salt doesn’t help. “Salt overconsumption can lead to hypertension, a serious risk factor for heart attack and stroke,” says Grace Ma, PhD, Director of the Center for Asian Health at Temple. Philadelphia’s nearly 400 Chinese takeout restaurants serve 9,000 customers a day. Like most take-out food, Chinese takeout can be high in salt. So the Center created the Philadelphia Healthy Chinese Take-out Initiative — a program teaching chefs how to cook with less sodium. Instead of salt, chefs are learning to use garlic, ginger, and other herbs and spices. They’re also reducing the amount of sauce they add to dishes. The American Heart Association recommends capping sodium intake at 2,300 milligrams per day. To date, more than 200 restaurants have voluntarily joined the initiative, which is funded by the Centers for Disease Control and Prevention. “The restaurant owners are very excited. They want to cook the right food for their customers,” says Steven Zhu, President of the Greater Philadelphia Chinese Restaurant Association — one of the groups collaborating with Temple, along with the Philadelphia Department of Public Health and the Asian Community Health Coalition. The restaurants have decreased sodium content in the range of 19 to 36 percent—a change that could improve health. And in a taste test, customers could not tell the difference.
4
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
Photograph by CLINT BLOWERS
At the Helm Michael Young, MHA, FACHE, has been named President and CEO of Temple University Hospital — taking lead responsibility for the clinical outcomes and financial performance of the 732-bed tertiary-and quaternary-care academic medical center. Young joined Temple University Health
YOUNG: PETER FREED; SPINAL CORD: MATT CLOUGH
Michael Young, MHA, FACHE
System’s management team in August 2018 as Chief Operating Officer. With more than three decades of leadership experience, Young is recognized for his ability to envision and develop market-responsive models of care delivery, in both urban and rural settings. “I build high-reliability, high-engagement systems with nationally recognized medical staff and management teams,” he says. A Fellow of the American College of Healthcare Executives, Young is a fourtime CEO: Pinnacle Health System (Harrisburg, PA); Grady Memorial Hospital (Atlanta, GA); Erie County Medical Center (Buffalo, NY); and Lancaster General Hospital & Health System (Lancaster, PA). For more about Young, see page 32.
Spinal Cord Injury: Promising News
A
fter a spinal cord injury, neurons in the brain must reconnect with neurons in the spinal cord in order for a person to regain use of a limb. But there’s a problem: The axons of mature nerve cells don’t regenerate. Now, however, this could change. Scientists at Temple discovered a naturally occurring protein that can kickstart regeneration. It’s called liver kinase B1 (LKB1). “LKB1 plays a role in neuronal development in the young, with levels sharply decreasing as we age,” says lead investigator Shuxin Li, MD, PhD, Associate Professor at Shriners Hospital’s Pediatric Research Center at Temple. “When we increased the level of LKB1 in an adult model of spinal cord injury, it stimulated long-distance regeneration in mature neurons — leading to significant gains in coordination
and movement,” Li says. In past research, Li identified specific peptides that also prompted neuron regeneration. Now he plans to test those peptides in combination with LKB1. “Together, these peptides and LKB1 could lead to the development of a drug that could be highly effective in helping patients with spinal cord injury regain function,” he says. The research, published in Molecular Therapy, was supported in part by National Institutes of Health and Shriners Research Foundation grants. Contributing researchers include scientists at Jichi Medical University in Japan. Each year, approximately 12,000 adults and children in the United States sustain a spinal cord injury. SUMMER 2019 | TEMPLE HEALTH MAGAZINE |
5
CURRENTS
Catchy Numbers NO. 1 In 2017 and 2018, Temple was number one in the U.S. for lung transplant volume — performing more lung transplants than any other medical center in the nation. TOP 5 PERCENT Jeanes Hospital has been named one of America’s 250 Best Hospitals (2019) by Healthgrades — placing it among the top five percent of more than 4,500 hospitals assessed nationwide.
Better Burn Care
TOP 10 PERCENT Fox Chase Cancer Center has been named a meritoriously performing hospital for surgical care — an achievement that places it within the top 10 percent of all hospitals evaluated by the American College of Surgeons.
ritical burn injuries put patients at risk for multi-organ failure, electrolyte imbalance, and sepsis,” says Lisa Rae, MD, FACS, Director of the Temple Burn Center. The Center, founded over 20 years ago and recognized by the American Burn Association and the American College of Surgeons, provides comprehensive in- and outpatient treatment for all types of burns, both minor and severe. At its hub is an intensive-care unit dedicated to patients with life-threatening burn injuries. These include partial-thickness burns affecting more
TOP 10 Temple University Hospital and Fox Chase Cancer Center were both top 10 finalists in the 16th Annual Delaware Valley Patient and Quality Award Program, organized by the Health Care Improvement Foundation to recognize hospitals and other providers in the Philadelphia region for innovation in advancing patient care.
“C 6
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
than 10 percent of the body; burns involving the face, hands, feet, genitalia, perineum or major joints; third-degree burns, electrical burns, and chemical burns; infected burns; and burns affecting the airways and lungs. “Our highly experienced team treats hundreds of burn injury patients each year,” says Rae, a member of the American Burn Association’s Advanced Burn Life Support course committee. Prior to joining Temple, Rae directed the Burn Surgical Fellowship Program at Vanderbilt University and served on the faculty of the Division of Trauma, Surgical Critical Care, and Burn Surgery.
DARIA KIRPACH
TOP 5 PERCENT Fox Chase Cancer Center has earned Press Ganey’s Guardian of Excellence Award (2018) for outstanding clinical performance. This award is given annually to organizations with sustained client satisfaction in the top five percent.
JAMES STEINBERG
Combating Cancer Disparities Despite advances in cancer prevention, detection, and treatment, minority populations bear a disproportionate cancer burden. But a $13.5 million National Cancer Institute grant could help change this. It’s been awarded to Temple University/Fox Chase Cancer Center and Hunter College of the City University of New York. “This funding creates a new coalition called the Synergistic Partnership for Enhancing Equity in Cancer Health (SPEECH) — which aims to reduce cancer health disparities in the Pennsylvania, New Jersey, New York City region — among African-American, Asian-Pacific-American, and Hispanic-American communities,” says principal investigator Grace Ma, PhD, Associate Dean for Health Disparities and Director of Temple’s NIH-funded Center for Asian Health. SPEECH has several aims: to deepen the understanding of the socioeconomic and cultural circumstances that lead to disproportionate cancer burden in minorities; to fortify the health disparities research workforce with investigators and educators who represent minority populations; and to establish a sustainable research infrastructure across the continuum of cancer care. Each year, only one or two such partnerships receive this federal funding. Temple is the first institution in Pennsylvania to be selected.
30-Year Puzzle Solved
T
emple researchers have identified something scientists have been trying to find for more than 30 years: the ligand that activates sigma-1 receptors in human cells. “Ligands are molecular connectors. They bind to different receptors in cells to activate various molecular processes,” says Eugen Brailoiu, MD, Adjunct Associate Professor at Temple’s Center for Substance Abuse Research (CSAR) and lead investigator of the paper announcing the discovery (Cell Reports, 2019). While endogenous (naturally occurring) ligands have been pinpointed for the vast majority of cellular receptors, it took more than three decades for researchers to identify the one that activates sigma-1. Perhaps researchers were on the wrong path.
“Sigma-1 receptors are the biological targets of psychoactive drugs. Therefore, many scientists suspected the endogenous ligand would be an opioid. But it’s not. It’s choline,” says Mary E. Abood, PhD, CSAR Professor. An essential nutrient, choline and its metabolites were known to fulfill important cellular functions. Now, with this new discovery, scientists will learn even more about choline’s roles. They plan to test other drugs and molecules that bind to sigma-1 receptors in order to better understand the choline pathway and the effects of sigma-1 activation. The research, a collaboration with the University of Cambridge and Thomas Jefferson University, was supported by the NIH and the Wellcome Trust.
A Marker for Jeanes, Who Made her Mark The Pennsylvania Historical & Museum Commission has approved 18 new state historical markers — including one honoring the Quaker abolitionist and activist Anna T. Jeanes (1822–1907). Jeanes’s legacy includes Jeanes Hospital in the Fox Chase section of Philadelphia and the Jeanes Supervisors program, which educated African-American teachers and students across the South. Other new state markers will honor singer/songwriter Jim Croce; Pulitzer Prize-winning author John Updike; and the Bethel Burying Ground, an early African-American cemetery.
SUMMER 2019 | TEMPLE HEALTH MAGAZINE |
7
CURRENTS
O
nly about eight percent of U.S. health care organizations have achieved Magnet® designation for nursing excellence — Temple University Hospital (TUH) among them. The designation was conferred early in 2019 by the American Nurses Credentialing Center following a vigorous review. “Magnet status is the highest form of recognition for nursing that can be achieved,” says CEO Michael Young, MHA, FACHE. “In addition to certifying nursing excellence
8
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
in every aspect of patient-care delivery, Magnet designation signifies a hospital’s commitment to community,” adds Elizabeth J. Craig, DNP, CRNP, FACHE, Chief Nurse Executive and Vice President of Patient Services. In 2018, Fox Chase Cancer Center achieved Magnet® designation for the fifth consecutive time. Symbolic of rigorous quality standards, Magnet® designation instills confidence in everyone who relies on a hospital and its nursing staff. For patients, physicians, and health professions students alike, it’s a real draw.
Stay Out of the “Pool” When portions of the heart are robbed of blood supply during an ischemic heart attack, heart cells die or lose their ability to contract. Ultimately this damage can lead to heart failure. But now Temple researchers have identified a new way to reduce the damage. It all centers on a molecule called G protein-coupled receptor kinase 2 (GRK2). “Following ischemia, GRK2 accumulates in mitochondria, the energyproducing powerhouses of cells,” says senior investigator Walter J. Koch, PhD, a GRK2 expert and the W.W. Smith Endowed Chair in Cardiovascular Research. “Now we know that blocking GRK2 can protect heart cells from dysfunction and death.” “Minimizing tissue injury helps the heart maintain better glucose metabolism, which is critical to maintaining contractility and overall function,” Koch explains. In addition to casting light on GRK2 as a potential therapeutic target for heart failure, the research also points to potential dietary influence on ischemic heart disease. Koch says GRK2 levels increase in mice on the high fat “western” diet. He suspects the western diet could be bad for heart health in people, too. The research, published in Science Signaling, was supported by the NIH, the American Heart Association, and the W.W. Smith Charitable Trust. Investigators from Drexel University and the University of MissouriColumbia contributed.
LJ DAVIDS
A Powerful Magnet
Duly Honored Sayed Ali, MD, Professor of Radiology, is one of five physicians
in Pennsylvania awarded Fellowship in the American College of Radiology in 2018. Just ten percent of member radiologists achieve this distinction. Mary Barbe, PhD, Professor of Anatomy and
Cell Biology, has been named a Fellow of the American Association of Anatomists, an honor recognizing scientists in the top 10 percent of anatomical sciences. She is also the recipient of the 2018 Research Prize of the International Society for the Study of the Lumbar Spine. Denise Connolly, PhD, Associate Professor,
Molecular Therapeutics, Fox Chase Cancer Center, received the American Cancer Society’s Philadelphia Scientific Research Award. Connolly studies ovarian cancer. John M. Daly, MD, FACS, FRCSI (Hon), FRCSG (Hon), is one of 91
surgeons from seven countries inducted into the inaugural group of the American College of Surgeons’ Academy of Master Surgeon Educators™. The honor recognizes mastery in surgical education. Emeritus Dean of Temple’s medical school, Daly is the Harry C. Donahoo Professor of Surgery and Surgical Director of the William Maul Measey Institute for Clinical Simulation and Patient Safety. Sara Feldman, PT, DPT, ATP,
Senior Physical Therapist, received the Allied Health Professionals Award of the International Alliance of MND/ALS Associations for her outstanding contributions to patient care.
JOSEPH V. LABOLITO
Arthur Feldman, MD, PhD, FCCC, the
Laura H. Carnell Professor of Medicine, received the American College of Cardiology’s 2019 Distinguished Scientist Award (Basic Domain) — recognizing “tremendous contributions to the cardiovascular field.”
Manish Garg, MD, FAAEM, FAIM, Professor of Emergency
Medicine, has been named President of the American College of Academic International Medicine, an organization advancing education, clinical productivity, and policymaking in international medicine. Steven R. Houser, PhD, Senior Associate Dean for Research,
received the Edward S. Cooper Award of the American Heart Association (Philadelphia chapter), recognizing contributions that “exemplify the best of humankind.” Houser was national American Heart Association President, 2016-2017.
Nirag Jhala, MD, Professor of Pathology and Laboratory
Medicine and Director Anatomic Pathology/ Cytology, has been named President of the Pennsylvania Association of Pathologists. Larry Kaiser, MD, FACS, the CEO of
Temple University Health System, has been named one of the 50 Most Influential Clinical Executives by Modern Healthcare. Kaiser is also Dean at the Lewis Katz School of Medicine and Senior Executive VP for Health Affairs at Temple University. Adil Khan, MSc, PhD, Associate
Professor of Pathology and Laboratory Medicine, has been named Chair of the Committee on Point-of-Care Testing by the International Federation of Clinical Chemistry and Laboratory Medicine. Jessica Kovach, MD, Associate Professor of Psychiatry & Behavioral Science, recently won the Outstanding Educator Award of the Philadelphia Psychiatric Society. Jacob Ufberg, MD, Associate Dean and
Professor of Emergency Medicine, has been selected to represent the Council of Residency Directors in Emergency Medicine on the national task force that defines the Emergency Medicine Model of Clinical Practice.
John M. Daly, MD
SUMMER 2019 | TEMPLE HEALTH MAGAZINE |
9
A Modern-Day Scarlet Letter Opioids have created the deadliest drug epidemic in American history. They killed more than 70,000 Americans in 2017 alone. That year, there were 5,456 overdose deaths in the Commonwealth of Pennsylvania. Most of them happened in a Philadelphia neighborhood called Kensington, a city neighborhood the federal Drug Enforcement Agency calls "the biggest open-air drug market on the East Coast." Kensington sits in the service area of Temple University Hospital's Episcopal campus. Its staff responds to as many as 15 opioid overdoses and related crises daily. “We’re ground zero,” says Larry R. Kaiser, MD, FACS, the CEO of Temple Health and Dean of the Lewis Katz School of Medicine.
By GISELLE ZAYON Illustration by MEGHAN WILLIS Photography by ANN CUTTING
10
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
G
iven Temple’s expertise in addiction medicine and population health, the Commonwealth of Pennsylvania, the City of Philadelphia, and other regional and national authorities seek its help in creating opioid response, prevention, and education plans. Temple Health has also established an opioid strategy of its own, a multidimensional plan that aims to permanently alter the treatment trajectory in North Philadelphia. “From groundbreaking research to prevention and intervention for those affected by the disease of addiction, Temple is doing its part to help combat this crisis,” says Pennsylvania Governor Tom Wolf, who declared the opioid epidemic a statewide emergency on January 11, 2018. This conversation with ten members of Temple Health’s Substance Abuse Task Force (see page 15 for full names and titles) reveals that addiction medicine in the United States has quite a way to go. Much hinges on combating the many myths that impede its progress.
Is opioid addiction a legitimate medical condition?
UNTERWALD: Yes. Addiction is a disease, rooted in biology. And
UNTERWALD: Most people dependent on opioids can’t get them
regularly. Therefore, they cycle between feeling “normal” and being sick, which wreaks havoc in the brain. MAT works by resetting brain chemistry, stabilizing it. The medication we use most often at Temple is buprenorphine (Suboxone®). Buprenorphine satisfies the opioid receptors in the brain, establishing neurochemical stability — which helps people create stability in their lives, freed from the nonstop quest to find drugs.
Unfortunately, only a third of addiction treatment programs in the U.S. offer MAT long term. Is this because of the stigma associated with the idea of treating drug addiction with drugs?
O’GUREK: Sometimes MAT is inappropriately referred to as
“substitution” or “replacement” treatment — which implies one opioid being substituted for another. This is a common misconception, even held by some in the recovery community. MAT is no different than any other medication for a health condition.
Is it true that only four percent of U.S. physicians are “waivered” to prescribe buprenorphine?
D’ORAZIO: Yes. Ironically, it’s harder to prescribe treatment for opi-
oid use disorder than it is to prescribe opioids. The DEA requires special training to be licensed (waivered) to prescribe buprenorphine. Since July 2018, Temple has focused on making sure more clinicians receive the waiver — and on mentoring newly waivered clinicians. We have helped launch office-based opioid treatment programs in numerous community practices outside of the Temple system, so that the needs of the community can be better met. MAT is only one aspect of treatment. It can be incredibly hard for patients to find a doctor trained to meet their full spectrum of needs. There are about 20 million people living with a substance use disorder in America, yet only about 5,500 physicians certified in addiction medicine. For years, psychiatrists were the only doctors treating addiction. Fortunately, the American Board of Medical Specialties recognized addiction medicine as a new subspecialty in 2016. This will help increase the number of physicians treating addiction.
more than half the risk is genetic. If you’re genetically predisposed for addiction and take a medically prescribed opiate, even for a relatively short time, you’re at high risk for developing an opioid use disorder. Last year, Temple and the Max Planck Institute identified more than 1,000 changes in the brain after a single exposure to an opioid. Some opioid-induced changes can be seen under a microscope. For example, with repeated exposure to opioids, dendrites wither. Dendrites are the “fingertips” of nerve cells that enable them to communicate with one another. Loss of connectivity impairs The year 2016 is also the year that cognitive function. addiction was finally officially Opioids acutely quiet the brain’s lodefined a chronic neurological cus coeruleus, the “stress center.” With disorder by the U.S. Surgeon repeated use, the brain becomes accusGeneral. Is stigma to blame — Joseph D’Orazio, MD tomed to the presence of opioids — and for the delay? super sensitive to their absence. When D’ORAZIO: Absolutely. Substance use disopioid levels drop, craving sets in, along with nausea, cramping, order rivals leprosy and HIV/AIDS among stigmatized condisweating, and shaking. The brain needs to re-establish what has tions. A federal study — also done in 2016 — showed that many become biochemically “normal.” The motivation to continue Americans believe that people with substance use disorders taking opioids is to avoid the distress of withdrawal, to simply feel should be denied housing, employment, social services, and well again. Substance use disorder is a chronic disease that can health care. Historically, Americans have viewed addiction as a require lifetime treatment. moral failing. Addiction is a modern-day scarlet letter. Let’s not forget: Many people with opioid use disorder were Medication-assisted treatment (MAT) is proven to cut first exposed through “legitimate” means, prescribed medicine. the death rate by half or more. How does MAT work? Ten years ago, to curb the problem, regulators started clamping
“Temple is striving to make the treatment of substance use disorder resemble the treatment of other chronic medical conditions, such as heart failure, COPD, and diabetes.”
12
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
We tend to think of opioid addiction as a problem affecting the homeless or the poor.
AL-KHATIB: The population we serve comes from all walks of
life. They are congregating in Kensington, but they’ve come from all over—some from rich, expensive neighborhoods. As one of our patients said, “We had good lives, good homes. But addiction is a demon.” Addiction is blind to social class, affecting every strata of society. People who suffered childhood trauma are especially vulnerable. The higher your ACE score, the higher your risk for addiction.
What is an ACE score and how can it predispose someone to addiction?
REEVES: An important study was conducted in 1998 called the
down on opioid prescribing. This had the unintended consequence of some people turning to heroin — which is easier to get and one-fifth the price on the street. In 2016, opioid overdose killed four times more people than guns and knives in Philadelphia — in part because fentanyl is being mixed into heroin. This powerful synthetic opioid is implicated in 84 percent of Philadelphia’s overdose deaths. Stigma is a barrier as real as any wall. It has a negative impact on health outcomes. If you have cancer or heart disease, doors will open for you. Not so much for addiction. Especially if you inject drugs. Temple is striving to make the treatment of substance use disorder resemble the treatment of other chronic medical conditions, such as heart failure, COPD, and diabetes. All are often lifelong, non-curable medical problems that are highly dependent on medications and behavioral change. As can happen in COPD, there are times when patients with substance use disorder medically decompensate and need further treatment and support to achieve remission. Temple is working to take away stigma and focus on medical treatment.
How is language part of the stigma problem?
O’GUREK: What is common parlance for a positive urine drug
test? “Dirty.” A negative test? “Clean.” Let’s avoid this kind of harmful terminology and use language to open doors. Don’t say “addict”; say “a person with substance use disorder” or “opioid use disorder.” Don’t use the term “drug habit.” Addiction isn’t a habit; it’s a chronic disease. Even the term “medication-assisted treatment” is stigmatizing. We would never consider insulin a “medication-assisted treatment” for diabetes; we just call it what it is: treatment. Language is powerful. It can reinforce stigma or reduce it. It can shape public opinion, influence policy. It’s big.
Adverse Childhood Experiences (ACE) Study. It looked at how 10 types of childhood trauma affect long-term health. Updated versions are still being conducted. The ACE study is based on a survey that asks adults about different problems they experienced as children — things like violence, homelessness, hunger, sexual abuse. You get a score for each hardship you check. The more adversity you experienced, the higher your ACE score, and the more apt you are to experience adversity as an adult. Most Americans (64 percent) have an ACE score of one, and 12 percent have an ACE score of four. But in Temple’s service area, 45.5 percent score 4 or higher. Scores at this level double or quadruple your risk for addictive disease. In other words, the ACE study taught us that addiction is a predictable, expected outgrowth of childhood adversity. UNTERWALD: ACE scores aren’t just numbers. They represent changes to the brain, and to genes via epigenetics, creating neurobiological susceptibility to addiction. Even witnessing trauma is a risk factor for addictive disease.
Does Temple have the solution to the opioid epidemic? CARSON: Addiction requires a collective response across mul-
tiple sectors, including health care, government, social services, and education. Partnership and collaboration among federal, state, city, and private agencies are key. In July of 2018, the Temple Center for Population Health was awarded a $1 million grant from the Commonwealth of Pennsylvania to develop an infrastructure to address substance use disorder. We have assembled comprehensive resources to address this epidemic — reaching out to community-based providers to help them offer services in their practices, and educating new providers in providing MAT. We are approaching addiction as a treatable disease, with coordinated strategies for prevention, harm reduction, treatment, support services, education, public health, and research. O’GUREK: There is no magic bullet for the opioid epidemic. No single model will be effective for everyone. You must deliver the right care at the right time and place based on what people want and need. We are looking at the problem from a comprehensive public health and community perspective, including the perspective of a person who developed addiction. AL-KHATIB: Our patients need different types of services. It would be impossible for someone in the grip of disease to put it all together. Therefore, Temple is collaborating with other providers to assemble services in a continuous flow. Our aim is to make services as complete as they can be and as easy to access as possible. We are establishing and renewing partnerships every day in order SUMMER 2019 | TEMPLE HEALTH MAGAZINE |
13
to provide our patients a more complete journey toward recovery. number of days that MAT is offered from two to five, thereby “Warm handoffs” help us catch individuals within that short windecreasing the wait time for new patient appointments from two dow of will for recovery. We don’t just give referrals. Whenever months a year ago to three business days today. We’ve standardpossible, we take people to the next level of care personally, introized warm handoffs from hospitals, emergency departments, and ducing them to the provider. Warm handoffs increase the chance other outpatient offices. Now that we have a solidified multithat seeking recovery will succeed. disciplinary team of addiction experts, patient flow is smoother CARSON: Part of our strategy is “internal,” mobilizing Temple’s and we’re able to engage patients in recovery more quickly. clinical enterprise in its entirety — and part of it is external, targeting agencies and community-based providers not employed by the In 2017 Temple launched Cease Addiction. Its goal is Temple Health system. With our partners, we have established to “interrupt” the spread of the opioid epidemic. five different interlocking programs for the Philadelphia commuWhat does this mean? nity — all funded in part by the Commonwealth of Pennsylvania REEVES: Substance use disorder is a preventable infectious and the City of Philadelphia. One program is Temple Recovery disease. Therefore, Cease Addiction uses the same tactics used Using Scientific Treatment (TRUST), an outpatient office-based by the Centers for Disease Control and Prevention to conopioid treatment program embedded in tain infectious epidemics. Step one: a city-wide network of medical and social Interrupt the spread. Step two: Treat services. Another is a Recovery Overdose affected people to help them recover Survivor Program, which connects from infection. Step three: Vaccinate patients who’ve survived overdose to cerunaffected people to help prevent them tified peer counselors who are in recovery from getting infected. We repeat these themselves. In addition, we launched a steps again and again. Comprehensive Opioid Respite Center Cease Addiction operates out of a van for patients who are homeless. that travels around Philadelphia neighHART: We also developed a streetborhoods. Our health outreach workers based outreach program called Cease come from the community. They’re Addiction and two programs for pregpeople affected by opioid use. This gives nant women and women of child-bearthem credibility, makes them worthy ing age, which are populations largely of trust. They mingle with folks in the underserved. One of these programs is community, trying to interrupt the use of a state-supported Center of Excellence. opioids. The goal is to connect them with D’ORAZIO: Certain tactics are essential treatment and support services. — David O’Gurek, MD in addiction medicine. We’re mobiTo “vaccinate” people from opioid lizing all of them: prevention; early use disorder, we start with elementary, identification of patients at risk for middle school, and high school children. addiction or already addicted; harm reduction for patients enWe teach them about ACEs. We provide services and support to gaged in substance use; pain management using non-addictive help prevent them from developing addictive disease. modalities; physician education and prescription monitoring — and tactics to reduce barriers to care and improve access to What else is Temple doing to reduce the risk treatment — including strategies to increase patient access to of opiate addiction? MAT. The Temple strategy for addiction medicine is a model of DEL PORTAL: In 2013, Temple became the first hospital in integrated initiatives aimed at permanently altering the trajecPhiladelphia to institute Emergency Department opioid pretory of substance use in North Philadelphia. scribing guidelines, promoting alternatives to addictive opioids for common minor conditions. We were also one of the first to TRUST is a large Temple, city, and statewide network establish an outpatient MAT program. of services. How does it work? What results have We’re integrating pain management education across the you seen? continuum of medical education, from medical students to VULGAMORE: TRUST is an office-based opioid treatment continuing medical education for physicians in the community. program within a medical network of agencies and experts. The idea is to approach pain management in new ways — to Together we address psychosocial support, transportation, minimize opioid use when there are safer alternatives. food, housing, peer recovery support, behavioral health, primaWe have developed guidelines and standardized order sets for ry care, social services, legal services, and vocational training. pain management for every one of Temple’s physicians in our Patients can start anywhere in the network and access everyelectronic medical record system. These guidelines differentiate thing the program has to offer. We identify and prioritize each between acute and chronic pain, and between ambulatory and patient’s unmet medical and social needs with a comprehensive inpatient settings. We limit dosing and supply. We use scheduled assessment — then create personalized treatment plans to link expiration dates for outpatient prescriptions. We follow best people to the care and support they need — complete with warm practices of the Centers for Disease Control, Enhanced handoffs guiding them through. Recovery After Surgery (ERAS) protocols, and Michigan We are just completing year one of the outpatient program Surgical Quality Collaborative guidelines. In surgery, we’re expansion — a year of infrastructure building. Within the last doing more perioperative pain management with NSAIDS, six months, we welcomed over 150 new patients, increasing the abdominal binders, nerve blocks, and other medications and
“Even the term ‘medication-assisted treatment’ is stigmatizing. We would never consider insulin a ‘medication-assisted treatment’ for diabetes; we just call it what it is: treatment.”
14
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
techniques that avoid or minimize opioid use. TREHAN: Our tactics are working. The total amount of opioids prescribed throughout Temple’s health system decreased by 45 percent from 2014 to 2017, concurrent with a 28 percent reduction in the number of opioid prescriptions written. The “opioid dashboard” we created in our electronic medical record system helped us achieve these results. It provides live feedback to physicians regarding opioid prescribing. Defaults are set in the system for daily morphine equivalence. If a physician is about to exceed the guideline, he or she will be notified immediately. This gives them the opportunity to think about dosage and quantity of medication prior to actually writing the script. The dashboard displays other information as well, including the physician’s opioid prescribing history, the frequency of the patient’s office visits, if a pain-management agreement has been signed, if urine drug screens have been obtained and their frequency, and other factors. Of course, we also use the national Prescription Drug Monitoring Program database to monitor patient compliance and to see if patients have obtained prescriptions from providers outside the Temple network. We are up front with patients about the opioid epidemic and the need for providers and patients to work together to contain it. We tell patients we’re using new and improved modalities to address pain. UNTERWALD: The Commonwealth awarded Temple the statewide contract to develop the curriculum for the safe prescribing of opioids for practitioners licensed by the state Boards of Dentistry, Medicine, Nursing, Optometry, Osteopathic Medicine, and Podiatry. We also worked with Pennsylvania’s Physician General to develop competencies and objectives for statewide medical student education for pain management and the diagnosis and treatment of substance use disorders. Temple is taking a lead role in educating providers nationwide on the appropriate use of opioids — for example, leading a national postgraduate course on opioid-sparing approaches to perioperative pain during a recent Clinical Congress of the American College of Surgeons.
Are Temple scientists working on developing new medications to treat opioid addiction? How about alternatives to opioids for pain?
UNTERWALD: Yes. Temple is one of 14 national Core Centers
of Excellence in the field of substance abuse and addiction research. In prevention, we’re studying the link between stress pathways and addiction. If we can pinpoint the biological basis for increased susceptibility induced by traumatic stress, that could help us develop preventive medication for people affected by trauma. We’re also working on novel treatment approaches. My colleague Dr. Mary Morrison’s study of clavulanic acid is in a phase I clinical trial. Another colleague is studying tetrahydropalmatine, which comes from a Chinese herbal medicine. We are investigating novel therapeutics to reduce craving and to help prevent relapse. In pain management, we are looking for ways to make lower doses of opioids work more effectively or to replace opioids altogether. We found two synthetic cannabinoids that enable low doses of morphine to achieve full analgesia, and another that shows promise of pain relief by itself. We’re also combining low doses of opioids with chemokine receptor antagonists to treat pain. As two of these are FDA-approved drugs, this line of
research should progress to the clinical stage more quickly. MAT is a developing field. In time it will be more nuanced. Patients at different stages of recovery need different medications. Acute withdrawal effects need to be treated one way, longterm maintenance of recovery another. There are many aspects of recovery that we need to target — as well as personalizing treatment for the individual patient.
Do academic medical centers have a special responsibility to advance addiction medicine?
Absolutely. We educate tomorrow’s healthcare professionals. Our research centers develop new diagnostics and treatments. Our primary responsibility is to translate knowledge into real change in the community. VULGAMORE: Temple is leading the way not just by collaborating but by openly sharing resources, data, and information with any agency that asks. This marks a monumental shift in strategy, from being protective of resources and intellectual capital to being open to working with all parties toward a unified goal. Opioid addiction is one of the strongest draws on the planet. An all-together, open-platform strategy must be adopted nationwide in order to overcome it. AL-KHATIB: We view ourselves as an academic community that engages in real time with the community it serves. Despite all the challenges, we will not give up. We continue to drive toward recovery. It is the responsible thing for Temple to do – an academic medical center at the epicenter of one of the biggest opioid crises in history. The path to prevention and recovery can be improved, simplified, and de-stigmatized. Temple is doing it. HART:
CONTRIBUTORS Yasser Al-Khatib, MBA, MSN, RN Associate Director of Nursing TUH-Episcopal & NE Campuses Nurse Manager, Crisis Response Center Steven R. Carson, RN, BSN, MHA Vice President, Clinical Integration Temple Center for Population Health Temple University Health System Daniel A. del Portal, MD, MBA Associate Professor, Clinical Emergency Medicine President, Temple University Hospital Medical Staff Joseph D’Orazio, MD, FAAEM, FACMT Director, Medical Toxicology, Emergency Medicine Assistant Professor of Emergency Medicine Director, Medical Toxicology Co-Medical Director, TRUST Laura Hart, MD Assistant Professor, Maternal-Fetal Medicine Director, High-Risk Obstetrics Clinic Director, Opioid in Pregnancy Center of Excellence
David T. O’Gurek, MD, FAAFP Associate Professor, Family and Community Medicine Co-Medical Director, TRUST Kathleen Reeves, MD Senior Associate Dean, Health Equity, Diversity and Inclusion Director, Center for Bioethics, Urban Health and Policy Professor, Clinical Pediatrics Gaurav Trehan, MD, MBA, DABMA Chief, Division of Acute & Chronic Pain Medicine Associate Professor, Clinical Anesthesiology Ellen Unterwald, PhD Director, Center for Substance Abuse Research Professor, Pharmacology Patrick Vulgamore, MPH Project Manager Temple Center for Population Health
For more information or to request an appointment with the Temple TRUST Clinic, call 215-707-1122.
SUMMER 2019 | TEMPLE HEALTH MAGAZINE |
15
E
Chasing Down Alzheimer’s Disease
very disease takes its toll. But Alzheimer’s disease gets personal, co-opting the cognitive capacities that make us us. It’s identity theft on a molecular scale. First the disease affects brain regions involved in memory. Then it moves on to areas responsible for language, reasoning, and behavior. It will disrupt brain-based processes of cellular communication, metabolism, and repair until a person loses his mind and, ultimately, life. The most common form of dementia, Alzheimer’s disease affects one in every ten people 65 and older — with more than 5.5 million Americans currently diagnosed. The number will triple in 30 years — with health care costs projected to exceed $1 trillion annually. “Which is nothing compared to the human cost,” says Domenico Praticò, MD, FCPP, an Alzheimer’s disease researcher at Temple whose findings have drawn the attention of Newsweek, USA Today, and other highprofile consumer outlets. By GISELLE ZAYON
Photo illustration by ANN CUTTING
16
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
“People with Alzheimer’s are our parents, siblings, and friends,” he says. “Disease cannot diminish their value. Ask any one of the 15 million family caregivers if what I say is true.”
Thief Hunt
D
irector of the Alzheimer’s Center at Temple (ACT) and the Scott Richards North Star Charitable Foundation Chair for Alzheimer’s Research, Praticò says there are multiple theories about what causes Alzheimer’s disease. Like the notion that it’s the result of infection by the varicella zoster (chickenpox) virus. Or that it’s caused by environmental stressors, energy dysregulation, or diabetes mellitus. Praticò believes they could all be true, to varying degrees. “No one fully understands what causes Alzheimer’s, but there’s no single culprit. It’s probably a combination of genetic factors with different environmental exposures — and the way our bodies react over time,” he says. While there’s no shortage of possibilities to explore, Praticò is primarily interested in studying the impact of modifiable environmental influences on brain health — things like sleep and diet. “We need to understand how lifestyle choices impact the brain, for better or for worse,” he says — quoting the ancient Latin aphorism mens sana in corpore sano, which means a healthy brain lives in a healthy body. Using cellular and animal models of Alzheimer’s disease, Praticò and his ACT team study the influence of specific variables on the brain. They introduce a variable and observe the reaction step by step — identifying the molecular players affected, deciphering their roles — hunting for targets for possible new therapies to prevent or reverse pathology along the way. Neuroscientists often discover things that are novel to brain science. The field is still new. Differentiating normal activity from abnormal can be tricky. After all, the agents in Alzheimer’s disease also have roles in normal brain physiology — including the amyloid beta plaques and tau protein tangles well-known in the disease. Inside neurons are little channels called microtubules. Nutrients and other elements travel through these microtubules from the center of the cell to the periphery. Normal tau maintains microtubule health and structural stability. But in Alzheimer’s disease, these channels collapse, turning into fibrotic, useless tangles. Normal tau protein has a certain structure. But in Alzheimer’s disease, a tiny portion of tau sticks out — that snags with other pieces of tau. The tangles pile up, eventually leading to microtubule collapse. Once a cell's intracellular transport channel is broken, all bets are off. The cell will suffer an energy shortage, irreversible dysfunction, then death. Good cellular health hinges on tau retaining its normal shape. “This is why Alzheimer’s disease is considered both a proteinmisfolding disease and a tauopathy, a pathology of tau,” Praticò explains.
Likewise, the amyloid beta protein that forms the famous plaques in Alzheimer’s plays a role in normal physiology too. At normal (low) levels, amyloid beta acts like a lubricant, maintaining consistent chemical connection between nerve cells. Basically, the protein helps brain cells communicate. But when the amount of amyloid exceeds normal levels, bits of it stick together, forming fibrils that hang around, disturbing cellular function. Eventually the fibrils harden into plaques that clog biochemical traffic, compromise blood flow, and keep nerve impulses from getting through. “When you consider that every neuron may have as many as 7,000 synaptic connections with other neurons, that’s a lot of messages lost,” Praticò says. “Yet by the time we realize something’s wrong, a surprising amount of damage has been done. This is how Alzheimer’s disease steals identity, molecular bit by insidious bit.”
New Signs
A
myloid plaques and tau tangles have long been considered the two classic hallmarks of Alzheimer’s. But a third sign has been recognized in recent years: neuroinflammation. “Inflammatory reactions are consistently found in the brains of patients with Alzheimer’s disease — and Domenico Praticò was among the first to recognize this,” says Sam Gandy, MD, PhD, the Mt. Sinai Endowed Chair in Alzheimer’s Research at the Icahn School of Medicine in New York. There could well be additional signs we’ll come to recognize as markers of the disease, Praticò says. One already coming to the fore relates to autophagy, the process that clears the brain of debris and toxins. “Autophagy is trash collection on the molecular level. It’s always dysregulated in Alzheimer’s,” Praticò says. Many things affect autophagy. Including what we eat. Last year, ACT conducted a study linking diet and autophagy that got people excited. After it was published in the Annals of Clinical and Translational Neurology, the news was quickly picked up by consumer media around the world. The study relates to the Mediterranean diet, long known for its beneficial effects on health. “We discovered that regular dietary intake of extra virgin olive oil — a staple of the Mediterranean diet — preserves memory and protects the brain against cognitive decline,” Praticò explains. “We proved that extra virgin olive oil has positive effects on autophagy.” In this study, mice engineered to develop Alzheimer’s pathology were put on a diet enriched with extra virgin olive oil at six months old, before symptoms of Alzheimer’s begin to emerge. At nine and 12 months, the mice were given tests to assess their memory and learning ability. They performed significantly better than the “Alzheimer’s” mice that had been fed a standard diet.
“We need to understand how lifestyle choices impact the brain,” Praticò says, quoting the ancient Latin aphorism mens sana in corpore sano, which means a healthy brain lives in a healthy body.
18
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
Under the microscope, brain tissue target with disease-modifying potenfrom both groups of mice revealed dratial for Alzheimer’s. matic differences. But here’s the take-home message: “One thing stood out immediately: The compound that ACT used doesn’t The synapses, the little connection just affect 12/15-lipo. It activates the points between nerve cells, were wellbrain’s natural waste-removal system: preserved in animals on the extra virgin autophagy. The extra virgin olive oil olive oil diet, but deteriorated in mice on worked the same way. the standard diet,” Praticò says. “In this exciting new study, the Why? Because the brains of mice on authors provide support for a new the olive oil-enriched diet showed a experimental treatment approach that dramatic uptick in autophagy compared works by helping nerve cells digest to mice on the standard diet. toxic proteins that might otherwise “This accounts for their lower levels of cause cell death,” said John Krystal, amyloid plaques and phosphorylated tau MD, editor of Biological Psychiatry, — and it is an important discovery, since which published the research in 2017. we suspect that a reduction in autophagy As exciting as this is, Praticò knows is really what marks the beginning of better than to quickly proclaim a cure. — John Krystal, MD, Editor, Alzheimer’s,” Praticò notes. “We must remember that autophagy The ACT team was very excited to see is a not a simple thing. Many things Biological Psychiatry a significant reduction in pathology in affect it. Many biological pathways are animals otherwise destined to develop involved — for example, the mammaAlzheimer’s disease. lian target of rapamycin (mTOR),” he says. “Stay tuned. Now we’re studying what happens when extra Basically, mTOR regulates cell growth and metabolism. virgin olive oil is introduced into the diet of mice that already Disruptions in mTOR have been implicated in cancer, have plaques and tangles,” Praticò says. “We want to know diabetes, and a number of neurological diseases — including whether adding the oil at a later time can stop or reverse the Alzheimer’s disease. disease. This is important since most patients are first diagnosed Praticò and team wanted to find out more about mTOR, to at advanced stages of pathology.” see how diet might affect it. So they fed mice destined to develop Can Alzheimer’s pathology really be reversed? Yes. ACT Alzheimer’s pathology a high-sugar diet — and found that debris proved it while studying a protein that is markedly elevated in and toxins are left behind in the brain. the brains of Alzheimer’s patients. It’s called 12/15-lipoxygen“Sugar, we discovered, activates mTOR,” Praticò explains. ase (12/15-lipo). And it elevates at an early stage, before sympPrior to this experiment, scientists knew that mTOR sigtoms begin to appear — making it a suspect in pathology. naling was somehow linked to the presence of amyloid beta plaques and tau tangles in the brain — but no one knew how. “Now a precise connection is known: sugar,” Praticò says. Full Reversal “Sugar activates mTOR signaling — which decreases autophagy. hile looking at the pathway of change to 12/15-lipo, In other words, we have learned that mTOR is a negative reguACT discovered something significant: that the lator of autophagy.” elevation of 12/15-lipo activates another enzyme There are drugs that block mTOR activity — which could called beta secretase-1. This is important because beta secreprove helpful. But as Praticò reminds us, sugar intake is sometase-1 is the principal player in the formation of the amyloid thing we don’t need drugs to control. beta plaques in Alzheimer’s. “So we wondered what would happen if change to 12/15-lipo What Mom Ate were blocked. Maybe that would keep beta secretase-1 from stimulating amyloid plaque buildup,” Praticò explains. ne risk factor for late-onset Alzheimer’s disease is not After finding a compound that blocked change to 12/15-lipo, well-understood nor widely known: Having a mother the team tried it on young mice destined to develop tangles with Alzheimer’s makes you four times more likely to and plaques. get it than having a father who did. “It worked. It prevented the onset of symptoms,” Praticò says. The logical cause would be genetic, something related to Then ACT tested the compound in mice with full-blown the X chromosome. Or to mitochondrial DNA, which, unlike Alzheimer’s brain pathology. Again, success. The compound nuclear DNA, we inherit entirely from our mothers. But these significantly reduced levels of amyloid beta and insoluble tau, possibilities have been studied. The answer is no. There’s no which in turn reversed cognitive decline. In fact, after three genetic link. months of treatment, the treated mice were indistinguishable So, what then? What is unique to women, Praticò poses? from normal mice in a memory test. Pregnancy. Perhaps something happens during pregnancy — “This study showed, for the first time, that selective pharsleep disruption? stress? — to increase the risk for offspring to macologic inhibition of 12/15-lipo can rescue the entire develop Alzheimer’s later in life. Alzheimer’s disease-like phenotype,” Praticò says. To find out if diet during pregnancy could be a predisposing These findings established 12/15-lipo as a novel therapeutic factor for Alzheimer’s — or a protective one — ACT scientists
“In this exciting new study, the authors provide support for a new experimental treatment approach that works by helping nerve cells digest toxic proteins that might otherwise cause cell death.”
W
O
SUMMER 2019 | TEMPLE HEALTH MAGAZINE |
19
Clue to Crazy Clue
H
eart disease has been linked to hyperhomocysteinemia. The amyloid beta plaques of Alzheimer’s have been associated with the condition, too. And last year, ACT became the first to link the condition to tau brain pathology. The study, published online in 2018 in Molecular Psychiatry, showed why: Diet-induced hyperhomocysteinemia upregulates (superactivates) the phosphorylation of tau protein. Phosphorylation is a normal biological process. But
Dr. Praticò (on left) with Antonio di Meco, PhD, a former graduate student who is now a postdoctoral fellow at Northwestern University
20
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
hyperphosphorylation is bad. It causes tau to detach from the cell’s microtubules, so it floats around inside the cell, snagging onto other bits of tau, forming those fibrous tangles. ACT made this discovery by putting one group of mice on a diet high in homocysteine, and another on a standard diet. “The mice on the high-homocysteine diet developed hyperhomocysteinemia, had 50 percent more tau tangles than mice on the standard diet, and performed significantly worse in tests of learning ability and memory,” Praticò recalls. During this research, the team discovered something else about high homocysteine levels. They activate a protein in the brain called 5-lipoxygenase (5LO). From previous research (Biological Psychiatry, 2015; Translational Psychiatry, 2017), ACT knew that 5LO controls an enzyme called cyclin dependent kinase 5 — which causes tau to hyperphosphorylate. In other words, 5LO is ultimately responsible for pathological tau. Now, to go a step further, Praticò discovered that 5LO is also responsible for making metabolic products in the brain called leukotrienes (Frontiers in Cellular Neuroscience, 2015). “Leukotrienes trigger an immune-cell inflammatory response surrounding nerve cells. At the onset, leukotrienes attempt to protect nerve cells, but over the long run — as happens whenever inflammation becomes chronic — leukotrienes do more harm than good,” Praticò says. While 5LO and its metabolites were known to control
EDWARD CUNICELLI
put one group of pregnant mice on a high-sugar diet, another on a high-fat diet. Not surprisingly, the sugary diet was bad news. The brains of the babies of sugar-fed moms were riddled with pathology. Alzheimer’s disease set in quickly. But the high-fat diet turned out to be beneficial for the offspring. It was protective for Alzheimer’s. “The hippocampus was a third bigger in pups born to mice moms on the high-fat diet. A bigger hippocampus is good for brain health,” Praticò says. Does this mean we should start eating fat? No. It’s good for the developing fetus, but that’s where it ends. In fact, diets containing a lot of red meat (and/or lacking in B vitamins) can lead to a condition called hyperhomocysteinemia (too much of the amino acid homocysteine), and this definitely is not good.
inflammation in other disease states, ACT was the first to determine that 5LO is also ultimately responsible for inducing aberrations in both amyloid beta and tau protein (Molecular Psychiatry, 2014; Annals of Neurology, 2012) and to determine that elevated homocysteine activates 5LO. With so much evidence pointing to 5LO as a troublemaker, ACT was now ready to find out if blocking 5LO could reverse nerve cell damage induced by high levels of homocysteine. And Praticò knew exactly how to block it: with an asthma drug developed two decades ago called zileuton.
An Asthma Drug?
“W
“Extraordinary things happen when scientists, funders, and patients come together in commitment to beating the odds. Alzheimer’s is a tricky identity thief, but I’m convinced we’ll catch it,” Praticò says.
e thought of zileuton because we knew that leukotrienes don’t work properly in asthma. Zileuton inhibits leukotriene formation by blocking 5LO activation,” Praticò explains. So ACT tested zileuton on mice with tau tangles. The results were reported online last year in Molecular Neurobiology. After 16 weeks of treatment, the mice were given maze tests to assess their working memory and spatial learning skills. The mice on zileuton performed significantly better than untreated mice. “Their superior performance suggests a successful reversal of memory deficits,” Praticò says. The mice treated with zileuton had a 90-percent reduction in leukotrienes and a 50-percent reduction in phosphorylated tau, compared with untreated mice. Moreover, the synapses of the mice on zileuton were indistinguishable from those of mice without the disease. The synapses of untreated mice, on the other hand, were severely deteriorated. “In mice treated with the drug, inflammation was completely gone in the brain. The therapy shut down inflammatory processes, allowing the tau damage to be reversed. It’s really dramatic,” Praticò says. As a bonus, previous research by ACT showed that zileuton also decreases amyloid pathology. “Best of all, zileuton is already approved by the Food and Drug Administration — which should give it a good head start toward clinical research in patients with Alzheimer’s,” Praticò says. “That’s the goal.”
North Star
A
homemade sangiovese from an old family recipe. His wine has not won any awards, but his research has. Praticò has been honored by the Alzheimer’s Association and the American Federation of Aging Research. He has 20 years of continuous NIH funding behind him, along with a book, 25 textbook chapters, 250 peerreviewed articles, and 27,000 citations by other scientists. In 2017, he was also named the Scott Richards North Star Charitable Foundation Chair for Alzheimer’s Research at the Lewis Katz School of Medicine. The North Star Charitable Foundation is the philanthropic arm of the North Star Resource Group, one of the largest financial service firms in the world. It was founded by Phil Richards, a Temple University trustee and 1962 alumnus. Alzheimer’s disease research is a stated interest of North Star’s charitable foundation. Therefore, supporting Praticò seemed only natural. “In my 60-year love affair with Temple University, making this gift to Alzheimer’s research at Temple is a crowning event on steroids for me,” said Richards during the celebration of Praticò’s installment as the Scott Richards North Star Charitable Foundation Chair. The name of the chair honors Richards’s late son, Scott, who was born at Temple University Hospital in 1962 and was North Star’s president before his untimely death in 2008. While North Star is ACT’s key private supporter, other private foundations back ACT, too. A foundation called Stop Alzheimer’s Now, for example, is funding a study of adult neurogenesis, the development of new neurons in the brain. This essential process all but stops in Alzheimer’s disease. Little is known about why. But thanks to the grant, ACT discovered an important clue: a protein that controls it. Perhaps this protein can be targeted to stimulate neuron growth. This would be a breakthrough. “The reason I funded ACT was simple,” says Shaun McDuffee, founder of Stop Alzheimer’s Now. “Dr. Praticò and his team. Their dedication, passion, and commitment to wiping out this disease are second to none.” Praticò revels in high-risk, high-impact work — and in the scientists he works with and the young scientists they train. Two of his newest colleagues are Miroslav Nenov, PhD, and Silvia Fossati, PhD. Nenov heads ACT’s electrophysiology laboratory. Fossati studies cerebral amyloid angiopathy — as well as traumatic brain injury and post-traumatic stress disorder — and their interplay with Alzheimer’s. “Extraordinary things happen when scientists, funders, and patients come together in commitment to beating the odds. Alzheimer’s is a tricky identity thief, but I’m convinced we’ll catch it,” Praticò says.
clinical pharmacologist from Reggio Calabria, Italy, Domenico Praticò, MD, FCCP, moved to the United States in 1994. With this move, he gave up practicing clinical medicine to devote himself full-time to his true passion: doing original research to help advance patient care. Initially he worked at the University of Pennsylvania. Since 2007, he's been at Temple, holding professorships in Pharmacology; Microbiology and Immunology; and in the Center for Translational Medicine at the Lewis Katz School of Medicine. When Praticò is not in the lab, he loves exploring Philadelphia's ethnic food scene with his family — and making
For more information about the Alzheimer's Center at Temple, visit medicine. temple.edu/alzheimers; to make a gift to ACT, go to giving.temple.edu/ givetotemplehealth SUMMER 2019 | TEMPLE HEALTH MAGAZINE |
21
Mai Stewart, MD: Drawings That Draw Big
DOCTOR Doo DLE M
ai Stewart, MD ’19, a brand-new graduate of Temple’s Lewis Katz School of Medicine, has been drawing illustrations about her life in medical school that have been blowing up on Instagram. She now has more than 18,000 fans and followers @maidoodles, and each drawing gets hundreds of likes. She also posts on her website, www.maidoodles.com. Each of these drawings is a story, a reflection on her experiences in medical school, and a way for her to process and share her feelings. She’s able to recognize what is often a universal feeling in medical school and express it cleverly, succinctly, whimsically, and effectively in an illustration, a comic. She has always drawn for fun. Then she got an iPad and began drawing on it. Friends urged her to post on Instagram, to share with the world, and one day she just took the plunge. Why did she draw about medical school? “Laughing at it was better than crying about it,” she says.
By MICHAEL VITEZ Photography by JOSEPH V. LABOLITO
SUMMER 2019 | TEMPLE HEALTH MAGAZINE |
23
When The Philadelphia Inquirer wrote about her last fall, journalist Tom Avril aptly called her humor “scalpel sharp.” “I’m very grateful to have experienced med school and have all the opportunities I have,” says Stewart, who grew up in Montclair, NJ, and Lancaster, PA. “But it’s still a difficult process. Everyone has moments, thinking ‘I just can’t do this’ or ‘It doesn’t make sense.’ Medical students understand it. But I’m not sure if people outside of medicine really can. “Nobody can really know what medical school is like until you go and do it,” she says. “Plus, I’m a very cynical person,” she adds. “I was born that way. I think if you were a positive person, there’d be no good comics. There’d be nothing to draw about.” Stewart also illustrates physiological processes. In one drawing, she depicts what happens to the heart when it infarcts. The practice helps her absorb and remember complex material — and her classmates benefited, too.
The Philadelphia Inquirer journalist Tom Avril aptly called her humor “scalpel sharp.”
She’s not sure who her audience will be now that she’s graduated and moved away to start her residency training in radiology — but she suspects she’ll start attracting other residents among her followers and perhaps continue to be followed by medical students and pre-med students. Many viewers comment on her drawings and sometimes she’s tempted to reply, but usually settles for a ♥ acknowledgement. “I feel like you never regret not commenting,” she says. These days she tries to do one or two drawings a week, though she probably has an idea every day. She says each drawing takes about two hours, but it’s rarely a linear process — often interrupted by sleep, studying, Netflix — so it’s hard to tell exactly how long. She plans each illustration carefully. “The actual drawing is the quickest part,” she says. Stewart draws a rabbit named Steve in many of her doodles, “but unfortunately he only hops about in the recesses of my imagination,” she says. “I’ve wanted a pet rabbit — but want to make sure it’s at a time when I can give it the care and attention it needs.” “I’m actually concerned about my life after medical school,” she says. “What I’ll even draw about. I’m sure residency will be significantly harder, and I’m sure there will be tons of fodder.” To see more of Dr. Stewart’s doodles, visit: www.instagram.com/maidoodles
24
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
SUMMER 2019 | TEMPLE HEALTH MAGAZINE |
25
INSIDE STORY
Stories of the Human Side of Medicine “ALONG WITH THE PHYSICIAN’S TOUCH, stories are at the
core of the patient-physician relationship,” says Michael Vitez, Pulitzer Prize-winning author and Director of Temple University’s Narrative Medicine Program. “Stories like these, written by physicians and students at the Lewis Katz School of Medicine, have the power to heal, inspire, build relationships, and change the world,” Vitez says.
Simply Call Him Abuelo The first day of February started like most winter Philadelphia mornings — cold, dark, and hurried. Rushing to the subway on my way to class as a first-year medical student, I called my parents to check on them. After an overnight snowfall, they were driving from their home in central Pennsylvania to their beach bungalow on the Outer Banks of North Carolina. Mom answered. She was waiting in the car at a gas station south of Harrisburg. Dad was taking a long time to come back from the bathroom. She was driving. Groggy and tired after working a 24-hour shift at the hospital, my dad had slept most of the trip. Luckily, the roads were cleared and salted and they expected to make Hatteras by nightfall. An hour later, I received a text from my mom asking if I had a moment to call. Lecture would be over at noon so I told her I’d call at lunch. “Can you call now?” Dad was in an ambulance. Moments earlier he noticed tingling and weakness in his left arm and had my mom pull to the side of the highway and call 911. I told her to head to the hospital and I would contact my siblings. My father is no stranger to tragedy. At 14, a transfusion-related acute lung 26
injury left him vented in the ICU. His parish priest performed last rites. Despite his physicians’ realistically dark expectations, he spent the next two weeks fighting back. When he was finally able to breathe on his own, he vowed to be the last child to receive a deathbed anointing of the sick. Now 60 years old, my father has spent four decades aiming to fulfill that promise, working as a pediatric intensivist at a large regional hospital. Four of his five children followed his path into medicine. He continually demonstrates Ralph Waldo Emerson’s assertion: “We acquire the strength we have overcome.” I called my brother Ken, a pediatrician in New York, and we drove together to Frederick, Maryland, along with his wife Monica and my fiancée Marissa. Hours later, on our frustratingly slow trip down I-95, we learned that my father had suffered a stroke but was doing well. The emergency physicians and neurologists had agreed to administer tissue plasminogen activator (tPA) when my father insisted the use of his nondominant hand was critical to continuing his life’s work. He was now alert and had regained strength in his left arm. Late that night, however, we arrived at Frederick Memorial to find a rapidly deteriorating situation. My somber father struggled as he described being
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
“imprisoned” in the intensive care unit. He lay prostrate upon the bed, attached to a catheter, despondent. His left arm was extremely weak and his face severely sunken. The stroke’s early resolution had all but reversed, and a significant hemiparesis had settled in. “He’s a max assist,” explained his bedside nurse, “he can’t help me at all with his left side.” When my sister Rosie arrived from Durham, we gathered around my dad’s bed. My mom had inquired about a priest, and he arrived to perform last rites, now the second time my dad had received the last breath sacrament. I looked to Marissa, and wondered if my father would live to see us married in July. My dad asked us all to come close, as if to offer his final earthly thoughts. He looked at my sister and then at me, and said “Abuelo.” Suddenly I realized that the stroke had affected more than just his pyramidal tracts. This brilliant physician and sharp-witted father was now simply uttering an irrelevant term in another language. I assumed the worst; this was the onset of a delirium precipitated by a growing intracerebral hemorrhage. My sister and I traded horrified looks. But then the entire dynamic changed literally in the blink of an eye. My father winked at my beaming brother, who then announced, “Moni and I are expecting a child. Dad is going to be a grandfather, an abuelo!” Ken had told my parents just the night before that Monica, a native of Argentina, was pregnant. Dad’s left side was almost completely paralyzed, his face drooped, legs and arms motionless. Amidst all this, his thoughts remained on his kids and their happiness. He smiled and closed his eyes. My father survived the night. There was no hemorrhage. There were no cognitive impairments. There were, however, many physical therapy sessions, stumbles, falls, and disappointments as he struggled to overcome a diagnosis of left-sided spastic hemiplegia. Support from the community poured in. Dear Dr. McKinley, Over the Easter weekend I heard the Illustrations by ANNA GODEASSI
unfortunate news that you had a stroke. As a stroke survivor myself, I knew what you were experiencing and began praying for you. Keep up the good work and keep hope alive. You probably don’t know my name but I’m sure you would recognize me. I’m the old lady with the cane who you often help going into church. Sincerely, M. Lloyd Throughout his arduous recovery, my father vowed to walk by my wedding day
and to hold his future grandchild in his arms. He progressed from a wheelchair, to crutches, a cane, and ever so slowly he began to walk. In July, my father stood proudly as Marissa and I exchanged vows. A few weeks later, his first grandchild was born, and the baby fell asleep in his arms. Six months to the day from his stroke, after proving to himself and his colleagues he was again skilled with critical care procedures, Dr. McKinley confidently walked through the double
doors of the intensive care unit and returned to his life’s work. Some may see him as a stroke survivor. Others as an inspiration. He is grateful to see himself as always: a physician. My family and I see him as all these things, and one more. We simply call him abuelo.
— TIMOTHY McKINLEY, MD ’19
Editor’s Note: This essay, which originally appeared in Neurology, February 13, 2018; 90(7), is reprinted with permission from the American Academy of Neurology.
SUMMER 2019 | TEMPLE HEALTH MAGAZINE |
27
24 Hours In the Epicenter One bitter day last winter, 22 Temple medical students chronicled their experiences at Temple’s Episcopal Hospital campus, the epicenter of response to Philadelphia’s opioid epidemic. These are excerpts.
3:52 a.m.
Single White Sneaker Medics had picked him up off the street, covered in his own vomit. The doctor looks in his pockets. No wallet, no ID. A plastic bag peeks out of his jeans pocket. I’m not sure what I thought heroin looked like. The small bag seems underwhelming. His breathing is agonal — slow, labored. The medical assistants remove his clothes, layers of sweatshirts over shirts. The doctor believes the patient has overdosed and orders Narcan. When the patient wakes, he is agitated, a sign that cocaine was combined with the heroin he injected. The doctor orders a benzodiazepine to calm him. Soon he rests peacefully. A nurse comes in to pick up his clothes. “His other shoe?” she asks, picking up the single white sneaker. “He just had the one,” the doctor replies, as if this is perfectly normal. The doctor crouches by the head of the bed. I kneel behind her. “What’s your name?” she asks. “How old are you?” No answer. “How long have you been using drugs?” Still no answer. “Have you been using your whole adult life?” Finally, a slight nod. “Have you ever been able to stop?” He shakes his head, no. “Do you have somewhere to live?” No response. “Where have you been sleeping, on the streets?” A nod. I don’t realize he’s crying until the doctor reaches her hand to gently wipe under his eyes.
— MIRANDA HASLAM MD Class of 2021
6:06 a.m.
The Missing Piece My life in medical school revolves around competition among my classmates. So, as I walk into the Crisis Response Center — where 13,000 people with mental illness (and often substance abuse issues) 28
come in crisis every year — I am struck by the calm. People in the waiting room are wrapped in blankets, many sleeping. The resident and I see our first patient, a man bent over almost 90 degrees. “Please, doc, help me,” he says, shaking. “I can’t be out there anymore.” My heart hurts for this man. It is cold outside. He is by himself in a crisis center in a neighborhood the Philadelphia mayor has declared a disaster area. “How are you feeling?” asks the resident. “Like I am dying. I don’t want to feel like this anymore.” I wonder what it feels like to die. I wonder if dying looks like the man in front of me. I wonder what I would do in his situation. The resident asks about his drug use and medical history. “Can you tell me your name?” The patient answers. “What city we are in?” The patient answers. “What month it is?” We wait in silence. “I can’t.” If I could, I would take out a small part of my heart and give it to him. We see more patients. For the next three hours, I forget about the grades that defined my life. I realize I had been losing the part of myself that wants to ask, “How did you get here, what are your dreams, who do you love?” — CAROLINE MACGILLIVRAY MD Class of 2021
11:00 a.m.
Disqualified The third patient I saw was young, homeless, and in crisis. He clutched a bag. “What’s in the bag?” asked the resident. “Just my lunch,” the patient replied. I had my doubts. “How long have you been using?” the resident asked. “More than 10 years,” he replied. “How long have you been homeless?” “My whole life,” he responded. He had tremors as well as fasciculations of his tongue — clear evidence of addiction. He pleaded that he wanted to “get better.” I was confident we could get him treatment. I was wrong. He was not taking anti-retroviral drugs prescribed to him for HIV. This disqualified him from rehab. We made an appointment for him to get his HIV drugs. “Less than a 50 percent chance that he makes that appointment,” the resident predicted.
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
The opioids that he wanted to stop were preventing him from accessing the HIV drugs that would keep him alive. This was addiction.
— AMBUJ SURI, MPH MD Class of 2022
3:14 p.m.
Naked
Al was eating his hospital lunch, a chili burger with slaw, about to be discharged after two days. He was an older man, gray hair. One minute, he said, he had been at the barber shop, and the next he was waking up at Episcopal. He blamed his diabetes. Al said he lived in Kensington in his own apartment. His family was back in Cleveland. He preferred to move around, live alone. When I asked about opioids, he let silence fill the room. Al finished his apple juice, put on a crew neck sweater. I thanked him for his time. A nurse wheeled him out the door. Turns out, Al is well known at Episcopal, brought in once a week, typically overdosed on heroin. This last time, paramedics found him on the street, naked. The hospital gave him the clothes he left in. Al was taken to a shelter, where the cycle would likely start again. Whatever I imagined an addict to look like, it was not Al.
— DANIEL YUSUPOV MD Class of 2022
11:01 p.m
Evolution “Over 50,000 patients come through this hospital a year,” an emergency department doctor tells me, “and it feels like 90,000 of them are involved with the opioid crisis.” On one recent eight-hour shift, they saw over 100 patients and 24 overdoses. The reason? The heroin was mixed with sympathomimetic drugs. It was called “Santa Muerte,” the Holy Death. “People screamed for nine hours straight, psychotic, hallucinating,” the doctor said. “Heroin barely has any heroin in it anymore.” How do we help with the drug crisis when the drugs are constantly evolving?
— ROSHNI BHAT MD Class of 2022
Answers I Won’t Get in Medical School
than their friends and family ever did
When friends and family ask about your new friends in medical school, How do you tell them that the people you know best are dead? That they died of lymphoma, renal failure, or dementia
Finding evidence of major life events: pacemakers, coronary bypasses, missing appendixes — or grossly inflamed lymph nodes in a body absent hair, A consequence of failed chemotherapy treatment
That every day they wait patiently on the brightly lit, pungent fourth floor To welcome curious students who withhold their emotions And wield stainless steel probes to learn more about them
How do you talk about hot pink fingernails on hands sliced open To unveil their hidden mechanisms? How do you explain that the woman on table 18 Has taught you as much as any of your
teachers, Despite never uttering a word, never moving a muscle, Never learning your name? How she brought together Six strangers who would not have been friends otherwise? How do you explain that without a room full of lifeless cadavers, Medical school would be more lifeless? How can you ever thank the woman on table 18? — CONNOR HARTZELL MD Class of 2022
SUMMER 2019 | TEMPLE HEALTH MAGAZINE |
29
QUEST
The Biology of Addiction Remember the 1980s television ads with an egg sizzling in a frying pan and the tagline, “This is your brain on drugs”? This public service campaign became a pop-culture classic — because of its brashness, not its scientific accuracy. Three decades later, we have a much better understanding of how drugs actually alter the brain, thanks to researchers like Ellen Unterwald, PhD, Director of the Center for Substance Abuse Research at Temple. In reality, Unterwald explains, drugs do not “fry” the brain — but do cause neuroadaptations in specific brain regions that are important for motivation, decision making, and impulse control. These are changes we can actually see on a molecular level. “Addiction happens when the brain becomes ‘normalized’ to the presence of the drug. Our goal is to develop therapies to re-normalize those changes, help stabilize people and get them on track to recovery,” Unterwald says. Unterwald studies addiction-like behaviors in mice and rats. She introduces them to a chamber with levers that, when pushed, enable them to deliver a drug to themselves at will. Their drug-seeking behavior will become increasingly compulsive because, over time, it takes more of the drug to produce a good feeling — and less time for the bad feeling of withdrawal to set in. Unterwald examines the animals’ brains to identify the biological changes implicated in these transitions. In one of her studies, Unterwald is looking for ways to decrease the cravings experienced by cocaine users attempting 30
to quit. Intense craving causes relapse. “Cravings are brain-based, physiological responses. And they can be triggered by anyone or anything a person associates with cocaine use,” says Unterwald, who has identified molecular targets in the brain linked to the craving response — and is testing different strategies using them to block craving. In these experiments, mice are conditioned to associate an environment with the feelings that cocaine produces. Later, they are re-exposed to the same environment so they will recall those memories and crave the drug. Unterwald then gives the animals an experimental drug targeting an intracellular signaling pathway in an attempt to disrupt the drug-linked memory. “The results show the mice no longer prefer the environment where they accessed the cocaine, suggesting that the drug memory has been erased,” she says. In related studies, tone and light cues are presented whenever a rat self-administers cocaine — so the animals come to associate those cues with the drug. Later, the rats respond to these same cues with
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
vigorous lever-pushing, indicating intense cravings — but when they are given the therapy used in the mouse study, the cues no longer inspire the drug-seeking behavior. Findings like this give Unterwald hope for progress in medication-assisted treatment for addiction. “Some people don’t think we should treat drug addiction with a drug, but it makes sense — and it works,” says Unterwald, who studies opiates and psychostimulants. While three FDA-approved therapies exist for opiate-use disorder so far, none is available for psychostimulants. “We need to help people with substance use disorders function while they work on other aspects of their lives — housing, jobs, families, relationships,” she says. This aids in the recovery process. Temple’s Center for Substance Abuse Research is a recipient of one of 14 NIHfunded substance abuse research Core Centers of Excellence grants in the U.S. Unterwald has been with the Center since its founding in 1998. She was named its director in 2008, when founding director Martin Adler, PhD, stepped down. The Center brings together 30 faculty representing 11 different science disciplines. “We’re passionate about preventing and treating substance use disorder,” she says. “Part of prevention is finding better treatments for pain. If we can treat pain with less addictive drugs, we will eliminate a lot of opioid dependence,” she explains. “Our Center’s strength is in our dedication to addressing this problem from multiple angles: improving pain treatment as well as treating people after they have developed a substance use disorder. Both paths are critical if we want to solve this deadly crisis.” Photograph by CARDONI
Ellen Unterwald, PhD
CHANGE AGENT
Michael A. Young, MHA, FACHE CEO, TEMPLE UNIVERSITY HOSPITAL
Q & A
As the Polish aphorism says, “A guest sees more in an hour than the host sees in a year.” You are new to Philadelphia and to Temple University Hospital. What do you see? I’m a five-time hospital CEO who has been in the hospital business for 30 years. I didn’t expect to be so impressed by Temple. But I am. I don’t think Philadelphians know what they have here.
Q: What do you mean?
A: Inside the business, Temple has a
stalwart reputation. Regionally, nationally — even abroad — Temple is recognized for its sophisticated expertise, the excellence of its technology, and the supremacy of its clinical staff. Physicians at the highest levels of medicine send their very sickest patients to Temple — patients with extremely complex problems. But people in the Philadelphia region may not think of Temple for their own care. Q: Why do you think that is?
A: Their preconceived notions about the
hospital don’t match reality. Most people in Philadelphia think of Temple as a hospital that treats poor people. And we do — along with patients in every other economic bracket. Here’s a tip: When you need health care, choose the hospital that treats the 32
sickest, most complex patients — and achieves outcomes that consistently match or exceed the national average. In Philadelphia, that’s Temple. There’s nothing that Temple cannot handle. Q: You say you want to transform how
Temple thinks of itself. A: Correct. Temple people tend to emphasize Temple’s mission of providing care to the underserved. That’s just the front door of the house. Let’s not forget to talk about what’s in the house: the full spectrum of specialty care — of unsurpassed quality — sophisticated facilities, Magnet-level nursing. We’ve got it all. Q: You’re known for resuscitating
financially struggling hospitals. In one case, it took you just one year to produce the first positive bottom line that a hospital had achieved in many years. How do you do it?
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
A: By looking at tiny details and the big
picture. By questioning things others do not question. By identifying opportunities others don’t see. Remember, “A guest sees more in an hour than the host sees in a year.” You have to look with fresh eyes. Q: Speaking of vision, you’re blind in one
eye. Has that been a detriment? A: If I could see with both eyes, you might be talking to a dentist right now, but vision problems made that impossible, so I pursued health administration instead. I got my Master’s in Health Administration at the University of Pittsburgh and did postgraduate work at Harvard — but being blind in one eye was an education, too. When you can’t see with both eyes, you lose perspective. Everything looks flat. So you must develop alternative ways of judging things. Perhaps my visual handicap gives me a unique ability to see new perspectives in health care. Q: You’ve led health care organizations in
four different states — practically rebuilding some from the ground up — and have achieved top-quality ratings. What’s your proudest accomplishment? A: Staying laser-focused on what patients need — and delivering it in unique ways, at high quality, to every market. To be successful, you must continually evolve and adapt to meet constituents’ needs. Q: You say there’s no job in Philadelphia
more important than leadership of Temple University Hospital. How so? A: Philadelphia would be in dire straits without the consistently reliable, superior care that Temple has provided to North Philadelphia for 125-plus years. If Temple suddenly closed, other hospitals simply could not step in to do what we do. There’s no substitute for Temple’s success, no alternative. Photograph by PETER FREED
GUTTER CREDIT HERE
Michael A. Young, MHA, FACHE
TOOLS OF THE TRADE
Respiratory Relief:
The Hemolung Respiratory Assist System
34
could potentially be mobile. Movement can help reduce the risk of ventilatorassociated pneumonia. “The Hemolung RAS could ultimately provide a safe, less-invasive alternative or supplement to intubation and mechanical ventilation,” says Criner, principal investigator at Temple for a clinical trial of the technology called Vent-Avoid. A pivotal trial to test the safety and efficacy of the Hemolung RAS, Vent-Avoid is the nation’s first clinical evaluation
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
of the Hemolung RAS process, which is known as extra-corporeal carbon dioxide removal. Thirty other hospitals across the U.S. are participating as well. A product of ALung Technologies (Pittsburgh, PA), the Hemolung RAS has been commercially available in Europe since 2013. “The Hemolung RAS could soon become an important tool in the United States for the treatment of acute respiratory failure in the intensive care unit,” Criner says.
Figure 1
Figure 2
JOSEPH V. LABOLITO
T
emple University Hospital is testing a new technology called the Hemolung Respiratory Assist System (RAS), a device designed to help patients experiencing severe flareups of chronic obstructive pulmonary disease (COPD). A condition affecting over 11 million Americans, COPD is the nation’s third-leading cause of death. The standard treatment for patients in acute respiratory distress is intubation and mechanical ventilation in a hospital intensive care unit. “This intervention is life-saving in most cases, but can also have side effects,” says renowned pulmonologist Gerard J. Criner, MD, FACP, FACCP, Chair of Thoracic Medicine and Surgery and Director of the Temple Lung Center. The complications of mechanical ventilation include collapsed lung (pneumothorax), alveolar damage, and ventilator-associated pneumonia. These complications are significant contributors to mortality in patients with COPD who are experiencing acute respiratory failure. According to Criner, reducing ventilator pressure can improve outcomes in critically ill patients — but low ventilator pressure can also lead to hypercapnic respiratory failure, the critical accumulation of carbon dioxide in the blood. “Carbon dioxide buildup can also result from COPD exacerbations themselves,” Criner says. This is where the Hemolung RAS comes in. The device is designed to remove carbon dioxide independently of the lungs by filtering it directly from the patient’s blood. This enables the ventilator to be set at a lower, safer pressure. Another advantage is that while mechanically ventilated patients are more bed-bound, patients undergoing treatment with the Hemolung RAS
HOW IT WORKS
The Hemolung Respiratory Assist System performs extra-corporeal (out-of-body) carbon dioxide removal. It works by routing the patient’s blood to the Hemolung cartridge, where carbon dioxide is removed, and then returning the blood to the patient. Special catheters carry blood from either the femoral or jugular vein to the machine, then back to the patient. The catheters are dual-lumen, meaning that they each contain two channels, one for blood flowing from the patient to the machine, and one for sending treated blood back to the patient. The catheter in Figure 1 is the femoral catheter. The Hemolung respiratory assist cartridge, Figure 2, performs the carbon dioxide removal. The cartridge consists of a combined gas-exchange membrane (composed of tiny hollow tubes) and a centrifugal pump. As blood moves through the device, “sweep gas” (room air) is pulled through the center of the tubes. The tubes are gas-permeable. Therefore, when the patient’s blood rotates around them, carbon dioxide molecules escape and float back out into the room. The treated blood is then routed back to the patient. As shown in Figure 3, a computer controls the device — enabling pump speed and sweep-gas rates to be set and carbon dioxide removal levels to be monitored in real time.
Figure 3
TIMELINE
Body of Knowledge
A Brief History of the Department of Anatomy and Cell Biology
T
emple medical school’s first “anatomy lab” (1901) was a modest hayloft in the stable where Samaritan Hospital’s horse-drawn ambulance was kept. But luminaries taught there — like Addinell Hewson MD, FACS (1855-1938), longtime secretary of the Pennsylvania Anatomical Board and editor of Holden’s Dissector (P. Blakiston, Son & Co., 1894). And Edmund W. Holmes, MD (18511905), who wrote Outlines of Anatomy: A Guide to the Methodical Study of the Human Body in the Dissecting Room (New Era Printing 1897, 1902). And then there was D. Gregg Metheny, MD (1873-1924), author, Dissection Methods and Guides (W.B. Saunders, 1914). Certainly, the accommodations for Anatomy and Cell Biology have come a long way. “Today’s 13,000 square-foot ultramodern teaching and research suite pairs digital technology and a 48-table gross dissection lab with dedicated space for clinical training and research,” says Steven Popoff, PhD, the John F. Huber Chair of the department. But that high bar set in 1901 for excellent teaching has stayed there. Several Temple anatomy faculty have gained international reputations over the years. “Fame or not, it’s the passion of Temple teaching that alumni can’t forget. Robert Troyer drawing with both hands at the same time, twisting balloons and rotating plastic bags while climbing a ladder to help students visualize the developing embryo; Carson Schneck, at 70, still jumping up on tables to demonstrate gait abnormalities,” Popoff says. Since 1969, Temple medical school graduates have rated Gross Anatomy among the highlights of their medical school experience — because, as the 1970 yearbook tribute to Carson Schneck says, the material was taught with “a clinical approach to what could have been just pure anatomic detail.” 36
More yearbooks have been dedicated to Anatomy faculty than to those in any other department. In the last decade alone, 21 teaching and research awards have been conferred on seven faculty (Mary Barbe, Mark Black, Nicole Griffin, Judith Litvin, Helen Pearson, Steven Popoff, and Arthur Washburn). Today, 10 Anatomy faculty teach students in Temple’s medical school as well as its schools of dentistry and podiatry — plus residents and fellows of Temple University Hospital. “And with more than $10 million in NIH funding, we’re continuing our tradition of research,” Popoff says. Current studies range from the underlying mechanisms of upper extremity musculoskeletal disorders (Barbe and Popoff ) to reinnervation of the bladder after spinal root injury (Ruggieri and Barbe) to research on a novel treatment targeting microtubule acetylation to treat
veterans with Gulf War illness (Black). Results of these and other studies appear in Bone, the Journal of Orthopedic Research, Clinical Anatomy, and other leading journals. Faculty also regularly contribute chapters to textbooks such as Interstitial Cystitis, 2nd Edition (Springer Nature, 2017) and Primer on Metabolic Bone Diseases and Disorders of Mineral Metabolism, 9th Edition (Wiley & Sons, Inc., 2019). “We give seminars all over the world, sit on grant review panels for the NIH, and review manuscripts for leading journals,” Popoff says, “but first and foremost, we teach. That’s our core mission.” Inspiration abounds. In 2015, Temple became the first medical school in the nation to use cadaver DNA to teach genetics to medical students, an educational innovation gaining traction among medical schools worldwide (JAMA, 2016).
1899
The Pennsylvania State Anatomical Board pays Temple $10 per month to store and distribute cadavers to schools of medical instruction in Pennsylvania.
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
1901
Temple’s medical school opens. Anatomy is taught in a stable loft. Teachers include Edmund W. Holmes, MD (Outlines of Anatomy: A Guide to the Methodical Study of the Human Body in the Dissecting Room, (New Era Printing 1897, 1902). In 1905, John B. Roxby, MD (1871-1957), becomes Chair of Anatomy.
Four of Anatomical Lore
In the 1940s and ’50s, numerous professional groups recognized John F. Huber, MD, PhD (1904 -1994), for his work with Chevalier Jackson delineating the bronchopulmonary segments. The Huber Lung Model (Clay Adams Scientific Company) was used nationally in medical education as a teaching tool for years. But it was student learning that most concerned “Daddy Huber,” as students fondly called him. In 1945, to improve the curriculum, he merged the departments of Anatomy, Embryology, and Histology — and ensured the faculty combined dissection with lectures in a “correlated” teaching paradigm. So beloved was Huber, who taught at Temple for 34 years, that he became the namesake of Temple medical school’s first fully funded endowed chair.
First to occupy the Huber Chair was J. Robert Troyer, PhD (1928-1993), who was famous for making homemade teaching models with shopping bags, rubber bands — anything lying around — to bring embryology concepts to life for his students. His passion for teaching was infectious. “To be a doctor means to be a teacher, and to be a teacher means to know how and when to listen,” said Troyer, who wrote yearly odes to the graduating classes in the medical school yearbook. In 1990, Temple established the J. Robert Troyer Award to recognize the graduating medical student with the highest GPA in courses taught by the department. Troyer taught at Temple for 40 years.
Carson D. Schneck, MD ’59, PhD ’65, a Temple alumnus who taught at Temple for five decades, inspired generations of students with his ability to memorize their names and his Socratic, animated teaching style. Schneck directed Gross Anatomy. Not satisfied with commercial textbooks, Schneck created Temple Gross Anatomy Notes. In 1960, he began “volunteering” to teach postgraduate courses to residents in PM&R, orthopedic surgery, and ENT — and continued for 51 years. He taught all over the world, accruing a bevy of honors, including the AOA Distinguished Teaching Award (1988). He wrote the paper that gave surgeons the basis for proper placement of lumbar screws and plates for spondylitic surgery and defined the diagnostic parameters for MRI imaging of the elbow, wrist, hand, knee, ankle, and foot.
During his heyday at Temple, Raymond C. Truex, PhD (1911-1980) — who’d earned international acclaim for denoting the sinoatrial and atrioventricular nodes and visceromotor innervation of the heart — was elected President of the American Association of Anatomists. A whiz of a teacher, Truex could weave utterly confounding details into a seamless whole that made sense to students. As editor of the 1959, 1964, and 1969 editions of Strong and Elwyn’s Human Neuroanatomy, he influenced entire generations of neuroanatomists. He taught at Temple from 1961 until the mid-1970s.
1922
Anatomy is now taught in the medical school building at 18th and Buttonwood Streets. The growing faculty includes D. Gregg Metheny, MD (1873-1924), author, Dissection Methods and Guides (W.B. Saunders, 1914).
1914
Addinell Hewson, MD (1855 -1938), joins the Anatomy faculty. Hewson is Secretary of the Pennsylvania Anatomical Board and editor of Holden’s Dissector (P. Blakiston, Son & Co., 1894).
TIMELINE
1930
Temple’s new medical school building opens at Broad and Ontario streets — with an anatomy suite featuring a dissecting room and space for lectures, research, embalming, and refrigeration — plus a museum of anatomy.
1936
John F. “Daddy” Huber, MD, PhD (1904 -1994), joins faculty, becoming Chair in 1944.
1988
Carson Schneck, MD, PhD, wins the national Alpha Omega Alpha/ Association of American Medical Colleges Award for Distinguished Teaching.
1997
1971
Raymond Truex, PhD (1911-1980), winner of the AMA Hoekton Medal (with Drs. C. P. Bailey, et al.) for contributions to the cardiovascular anatomy, is named President of the American Association of Anatomists. In 1978, J. Robert Troyer, PhD, becomes Chair of the Department, and in 1985 is named the inaugural John F. Huber Chair.
38
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
Steven Popoff, PhD, is appointed Huber Professor and Chair. In 2004, five Anatomy faculty are named to the inaugural group of Temple University faculty honored for impressive records of funded research.
1945
Huber is honored by the AMA for delineating the bronchopulmonary segments with Chevalier Jackson, MD, and Charles Norris, MD. In 1954, J. Robert Troyer, PhD (1928-1993), joins the faculty. In 1957, the Clay Adams Scientific Company creates the Huber lung model for teaching.
1963
Esther Greisheimer, PhD (1891-1982), and Troyer rewrite the 8th edition of Physiology and Anatomy, with Practical Considerations (Lippincott, 1963). Carson D. Schneck, MD ’59, PhD ’65, joins faculty in 1960, becoming Gross Anatomy course director in 1969.
2009
Temple’s $63 million new medical school building opens, with a Gross Anatomy suite named in honor of Carson Schneck that features a 48-table gross anatomy lab, a 30-seat glass-enclosed demonstration/conference room, and a clinical training/research facility.
2018
Mary Barbe, PhD, FAA, Professor of Anatomy and Cell Biology, wins the research prize of the International Society for the Study of the Lumbar Spine.
2015
Temple is the first medical school in the nation to use cadaver DNA to teach genetics to first-year medical students, an educational innovation gaining traction around the world.
BLACK & WHITE PHOTOS: MEDICAL SCHOOL YEARBOOKS; COLOR PHOTOS: COURTESY OF STEVEN POPOFF, PHD; LUNG: COURTESY SLIDESHARE.NET
IMPACT ALUMNI UPDATES
PHILANTHROPY NEWS
PARTNERS IN PROGRESS
Embracing the Unexpected
W
ant to hit a home run in medical education? Call someone in left field, like Bill Giles, the honorary president of the MLB National Baseball League and former chair of the Philadelphia Phillies. That’s what Sandra Harmon-Weiss, MD ’74, FAAFP, would advise. She’s immediate past chair of the Lewis Katz School of Medicine’s strategic advisory group, its Board of Visitors. “Bill was on the Board of Visitors in 2007,” Harmon-Weiss recalls. “Temple was designing its new medical school at the time — and it was Bill’s idea to curve its stunning glass façade, reminiscent of a stadium. The medical school is the most striking building for miles in any direction.” Years of board service to Temple and other organizations have taught Harmon-Weiss that experts in fields outside your own can help you really hit it out of the park. “Diversity is a catalyst,” says Helene Pavlov, MD ’72, FACR, who took over as Board Chair in July. “When you can put people with different vocations together, it can spark great and revolutionary ideas. And that’s what the Board is about.” Since its founding in 2004, the Board of Visitors has included physicians, of course, but also inventors, finance experts, startup specialists, and authors. They come together to advise the school, to sustain its distinctive edge. Pavlov says the school was distinctive from the moment it opened in 1901. It was a night medical school that admitted women. Unprecedented. “Temple is the unheralded, taught us to do the unanticipated, and to become the unpredictable and the unexpected,” she says.
highly sought-after musculoskeletal imaging fellowship at the leading center for orthopedics, the Hospital for Special Surgery in New York — which appointed her to join its staff following her fellowship – and named her Radiologist-in-Chief in 1997. She exceled in this position for 16 years. She was appointed Professor of Radiology in 1990 and Professor of Radiology in Orthopedic Surgery in 2001 at the Weill Medical College of Cornell. Through ingenuity and perserverance, Pavlov blazed a trail to sports medicine, and became an internationally recognized authority in sports medicine in both the radiologic and orthopedic circles. She developed radiologic platforms on which orthopedic surgeons depended for confirmation of diagnosis. Her books — including The Running Athlete: Roentgenograms and Remedies (Year Book Medical Publishers, 1987); Atlas of Knee Menisci: An Orthopaedic Pathologic Correlation (Appleton Century Crofts, 1983) and An Orthopaedic Guide to Plain Film Imaging (Thieme, 1999)— are orthopedic and radiologic reference staples.
“Drs. Pavlov and Harmon-Weiss are super-promoters. They advance the welfare of every organization they touch,” says Larry Kaiser, MD, FACS.
W
A BIT OF “HERSTORY” hen the astute and energetic Pavlov was about to graduate from Temple in 1972, she had every qualification to pursue her field of dreams, orthopedic surgery, and focus in the just-developing subspecialty of sports medicine. There was, however, just one problem: Orthopedics wasn’t quite open to women in those days. Uncertain of the future acceptance of female surgeons, she specialized in radiology, and secured a 40
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
Along with orthopedic surgeon and sports medicine pioneer Joseph Torg, MD ’61, Pavlov conducted a 30-year longitudinal analysis of cervical spine injury patterns in athletes. This game-changing contribution was thrice recognized with national awards from the American Academy of Orthopedic Surgeons and other high-ranking organizations. Perhaps most coveted, membership in the American Academy of Orthopedic Surgeons was granted to Pavlov in 1998. Harmon-Weiss likewise attained heights unexpected for women. After receiving her MD in 1974, she established a solo family practice in suburban Philadelphia, concurrent with a management position at the Family Practice Center at a local hospital and a faculty position at Temple — during which time she achieved Diplomate status in the American Board of Family Practice. “Still, I wanted to make a greater impact,” she recalls.
Helene Pavlov, MD (left), and Sandra Harmon-Weiss, MD
Ultimately — at the highest ranks of the health insurance industry — she’d do just that. During the 1990s through the early 2000s, Harmon-Weiss was Vice President and Head of Government Programs for Aetna U.S. Healthcare — managing government contracts that brought in billions in premium revenue. Her position gave her entre to groups penning national policy. She testified before Congress on behalf of the Health Insurance Association of America — the nation’s leading health insurance trade association at the time, representing more than 265 companies serving 110 million Americans. “I got the principal voice I wanted — not the voice of the insurance industry, but the voice of patients, especially the underserved,” she says. “Temple and its patients are never far from my mind,” says Harmon-Weiss, who also chairs the Temple University Hospital Board and serves as a Temple University trustee.
CARDONI
T
SUPER-PROMOTERS he Department of Health and Human Services, the Society for Medical Jurisprudence, and two-dozen other assemblies have benefited from Harmon-Weiss and Pavlov’s leadership and expertise. Therefore, patients have also. “Drs. Pavlov and Harmon-Weiss are super-promoters. They advance the welfare of every organization they touch,” says Larry Kaiser, MD, FACS, the Lewis Katz Dean at the School of Medicine and President and CEO of the Temple University Health System. The two are also among Temple’s most accomplished alumni, both recipients of the Katz School’s most prestigious honor: the
Henry P. and M. Page Laughlin Alumna of the Year Award. Kaiser calls them “model alums, physicians, and Board chairs.” A think tank for strategic positioning, the Board of Visitors concentrates on program development, curricular innovation, and growing the school’s research enterprise. Members connect the school to the private business community, foundations, and individual philanthropists for funding opportunities — yet Nina Weisbord, the school’s chief development officer, says the school’s most generous benefactors are the Board members themselves. Harmon-Weiss, for example, established the Emma C. Weiss Memorial Scholarship, an endowed scholarship for medical students planning careers in primary care. E. Ronald Salvitti, MD ’63, the chair preceding Harmon-Weiss, established three scholarships for the school. As a group, the Board created an endowed scholarship of its own: the Lewis Katz School of Medicine Board of Visitors Endowed Scholarship. A service-oriented medical student in the class of 2020 named Eric Curran is its first recipient. He volunteers with groups like HERO (Help Energize and Rebuild Ourselves) and the Temple Emergency Action Corps — “which was established in 2007 by William Greenfield, MD ’69, a member of Temple’s Medical Alumni Board — another group essential to our progress,” Kaiser says. Curran has already been published in the New York Times. “If that’s any indication, he will excel brilliantly and help change the future of medicine for the better,” Pavlov says. “That’s our job on this Board — to help the school excel brilliantly — by supplying creativity, connections, and capital in order to help Temple medical students and faculty continue on as our finest ambassadors.” SUMMER 2019 | TEMPLE HEALTH MAGAZINE |
41
Unfocused By EUGENE N. MYERS, MD’60, FACS, FRCS EDIN (HON)
I
TAXI DRIVER n 2018 to honor my dad — Barbara and I endowed the David Myers, MD, Professor and Chair in Otolaryngology-Head and Neck Surgery at Temple’s Lewis Katz School of Medicine. Our gift will also expand the department’s research platform and establish a leadership curriculum for ENT residents, along with a lecture series and resident research award in my dad’s name. Life truly is a matter of focus. My dad became a pioneer in otolaryngology — despite the fact that one of his high school teachers predicted he’d never do more than drive a cab. My paternal grandparents had come to America in 1902 as penniless newlyweds who fled their small Romanian village. Emperor Franz Josef was drafting men into the Austrian Cavalry, and my grandfather was having no part of that. Instead, he and his bride, who was a seamstress, boarded a steamship to the new country and opened a tailor shop in South Philadelphia. My dad, born in 1906, was their first child. Four more followed. My grandparents handled fabric with surgical precision — but spoke no English. This cast my dad into the role of family 42
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
Top: David Myers, MD ’33; Left: Cecelia Schmalbach, MD, MSc, FACS, the David Myers, MD, Professor and Chair in OtolaryngologyHead and Neck Surgery, and Eugene N. Myers, MD ’60, FACS, FRCS Edin (Hon).
spokesperson and translator at a very young age. It couldn’t have been easy, since until Dad went to grade school, he spoke no English himself, only Yiddish. Somehow he managed to graduate from the University of Pennsylvania and Temple’s medical school (1933). As predicted, he did drive a taxi — to pay tuition. Following graduation, he interned at Temple University Hospital. Interns rarely left the hospital and were forbidden to get married. Dad, of course, secretly married his sweetheart Rosalind Nicholas anyway. After internship, he worked as a preceptor in the downtown office of Dr. Matthew Ersner, Chief of Otorhinology, and operated with him at Temple University Hospital — and to support our family, he opened a general practice in our South Philadelphia row house. But this was 1933, the Great Depression. Dad’s patients paid their bills with homemade spaghetti sauce and pastry. Fortunately, my mom’s dad, Dr. Samuel Nicholas, visited us every week and left money in the fruit bowl on the dining room table, enabling our family to survive — and giving Dad enough cash
DAVID MYERS: COURTESY EUGENE MYERS; SCHMALBACH AND MYERS: DANIEL BURKE.
M
y grandfather was a general practitioner in South Philadelphia, my father was Chair of Otorhinology at Temple, and three of my uncles were physicians. I was born into the profession — but at the University of Pennsylvania, I majored in varsity athletics and drinking beer at Smokey Joe’s. I was, as they say today, unfocused. But after graduation, I met Barbara, a student nurse at Mt. Sinai Hospital in South Philadelphia. After her 3-to-11 shift, I would meet her for late supper in the hospital cafeteria with a group of nurses and house staff. After a few of these sessions, I realized the interns and residents weren’t any smarter than I was. If they could become doctors, then I could, too. Only one thing was lacking: the desire. At about the same time (circa 1955), Dr. Samuel Rosen, a preeminent New York otologist, visited Philadelphia to tell my dad about the stapes mobilization, a procedure he had devised. It was a 20-minute operation done through the ear canal under local anesthesia — which restored hearing to patients with otosclerotic deafness. It seemed like a miracle to me, and I wanted to be in this miracle business. When I shared these thoughts with my dad, he went right to Temple’s dean, Dr. William Parkinson, who said, “Tell Gene to take the necessary science courses, and we’ll admit him next fall.” I took the courses, married Barbara, who offered great encouragement, enrolled in medical school — and my life has been in focus ever since.
to travel to New York on occasion to visit Dr. Julius Lempert, an ENT pioneer who taught him the fenestration operation for otosclerotic deafness. (Fenestration was later replaced by Rosen’s stapes mobilization — and later by the stapedectomy.) Dad was a visionary and his energy and leadership did not go unnoticed. In 1955, Dr. Parkinson appointed him Chair of Temple’s Department of Otorhinology — and Dad transformed it into a full-fledged ENT service within five short years. He expanded the research effort. He created the otolaryngology residency program. I remember physicians coming in from Brazil and Australia to learn the stapedectomy from Dad. This man, who came from so little, went on to earn American Board of Otolaryngology Diplomate status. “David Myers was responsible for bringing the modern practice of Otolaryngology to Temple, and his leadership and vision
both experienced what it is like to be the “outsider.” My father was one of the first Jews appointed to an academic chair at Temple; Dr. Schmalbach is one of the first females. These are the thoughts that came to mind during the David Myers Chair ceremony, listening to Dr. Kaiser call our gift “transformational,” listening to all the magnificent things the speakers said — including Brian Burkey, MD, Vice-Chair of the Head and Neck Institute at the Cleveland Clinic Foundation, a longtime colleague of Dr. Schmalbach. When Dr. Schmalbach took the lectern herself, accepting the David Myers Chair, she described herself as “honored and humbled.” I felt exactly the same way. She said she knew that the best way to thank us will be to promote the Temple brand and to educate future leaders of otolaryngology. Indeed, her remarks were wonderful, and she is wonderful. But I must confess that the words that touched me most deeply were spoken by the Alando J. Ballantyne Distinguished Chair of Head and Neck Surgery at the University of Texas MD Anderson Cancer Center. His name is Jeffrey N. Myers, MD, PhD. He is our son. So in addition to honoring my dad, the David Myers Chair does something more. It is a thank you to Temple for supporting my dad’s quest to become a doctor. And my quest to become a doctor. In fact, it is a big thank you to Temple for educating seven doctors in the Myers family. Next year when my grandson Keith (Jeff’s son) graduates, he will have the distinction of being the fifth generation of doctors in our family, the eighth doctor in our immediate family, and the third generation of Myers Temple medical school graduates. All of this flooded poignantly into focus while I listened to Jeff talk about growing up watching me and my dad work long hours in medicine — followed by more hours together talking about medicine. “It never seemed like work — and this is what inspired me to become a doctor,” he said. He’s right. It isn’t. It’s love.
In addition to honoring my dad, the David Myers Chair is a thank you to Temple for educating seven doctors in the Myers family. can still be seen in our present-day program,” said Larry Kaiser, MD, FACS, the dean of the Lewis Katz School of Medicine and CEO of Temple University Health System, on the day Temple celebrated the chair we established in Dad’s name. I knew Dad had created a lasting legacy. But to hear other people talk about it made my heart jump with joy.
F
VIVID IN MY MIND’S EYE riday, October 23, 2018, the day we celebrated the David Myers Chair at Temple, was part ceremony, part family reunion, and all golden. And what a joy to see Cecelia Schmalbach, MD, MSc, FACS, a world-class physician Temple identified during a national search, installed as the first David Myers Chair. A talented microvascular surgeon and expert in cutaneous cancers of the head and neck, Dr. Schmalbach is the Deputy Editor of Otolaryngology-Head & Neck Surgery. She’s held leadership roles in major professional associations. She’s also the only head and neck surgeon in the North American HPV Working Group. Prior to accepting the Myers Chair, Dr. Schmalbach was Division Chief of Head and Neck Surgery at the Indiana University School of Medicine. Before that, she served in the United States Air Force. She was Division Chief of Microvascular Head and Neck Surgery at the San Antonio Military Medical Center. During Operation Enduring Freedom, Dr. Schmalbach served a two-year deployment in Afghanistan. Five major medals laud her service there — including the United States Air Force Meritorious Service Medal. She is also the recipient of high-level civilian honors. Of course, Dr. Schmalbach and my dad never met, but fate binds them. They both know the horrendous injuries of war. From 1942 to 1946, Dad served in New Guinea, the Philippines, and Japan in the Army Medical Corps, repairing facial war wounds. Also, they
ABOUT THE AUTHOR Distinguished Professor and Emeritus Chair of Otolaryngology at the University of Pittsburgh, Eugene N. Myers, MD ‘60, FACS, FRCS Edin (Hon.), is internationally known in otolaryngology-head and neck surgery. A clinician, author, researcher, teacher, and leader, Myers has elevated the practice of the specialty throughout the world. He is one of the two original editors of the textbook Cancer of the Head and Neck, now in its 5th edition, and has been president of all five major societies in the field — including the American Board of Otolaryngology-Head and Neck Surgery. Twenty-five of his former trainees are now chairs at academic institutions throughout the world. A Diplomate of the American Board of Otolaryngology and Honorary Fellow of both the Royal College of Surgeons of Edinburgh and the Royal Society of Medicine in London, Myers is recipient of the Distinguished Service Award of the American Academy of Otolaryngology and the Gold Medal for International Otolaryngology. He was the Lewis Katz School of Medicine’s 1995 Alumnus of the Year. SUMMER 2019 | TEMPLE HEALTH MAGAZINE |
43
SO NOTED
“Strategic investment in Temple will pay dividends to society for generations to come.” — LARRY R. KAISER, MD, FACS, CEO AND DEAN
“Medicine is now the infinitely broad relationship between the entire community and the medical profession — engaged together in discovering and removing the cause of disease.” — SAID IN 1930 BY JOHN B. ROXBY, MD, PROFESSOR OF ANATOMY
In its 2019 “America’s Best Employers by State” list, Forbes magazine named Temple University Hospital one of Pennsylvania’s best employers. TEMPLE UNIVERSITY HOSPITAL, 2018:
130,530
“We are really amalgams of the imprints made upon us by other people.”
TRAUMAS
11,547 PSYCH CRISES
14,677 SURGERIES
347
ORGAN TRANSPLANTS
300
BURN CENTER PATIENTS
2,488
BABIES DELIVERED
44
No. 1
in the U.S. for lung transplant volume.
“Science must move forward. The word ‘end’ doesn’t apply.”
“RECEIVING A SCHOLARSHIP HAS REINFORCED MY SENSE OF ALTRUISM.”
— DOMENICO PRATICÒ, MD, FCPP, THE SCOTT RICHARDS NORTH STAR CHARITABLE FOUNDATION CHAIR FOR ALZHEIMER’S RESEARCH
— DAVID DUGUE CANDIDATE, MD CLASS OF 2021
— CARSON SCHNECK, MD ’59, PHD ’65, EMERITUS PROFESSOR
EMERGENCIES
2,360
In 2017 and 2018, Temple was
“Passion must lead to good policy.” — TONY REED, MD, CHIEF MEDICAL OFFICER, TEMPLE UNIVERSITY HOSPITAL
In 2018, the Centers for Disease Control and Prevention granted Temple’s Diabetes Prevention Program “CDC Recognition Status,” signifying the program’s adherence to rigorous federal standards.
| TEMPLE HEALTH MAGAZINE | SUMMER 2019
ARTFUL ENDING
CHONGGUANG CHEN
An Undersea Story? This turtle-like creature is a sagittal section of a mouse brain. The laboratory of Lee-Yuan Liu-Chen, PhD, studies them to learn more about opioid addiction. She’s a professor in Temple’s Center for Substance Abuse Research. “The brain contains opioid receptors. One type is called the kappa opioid receptor (KOPR). With long-term use of opioids, alcohol, cocaine, nicotine, and other drugs of abuse, KOPRs and the systems
they activate become overstimulated — setting off anxiety and craving for more drugs,” says Liu-Chen. “Thus, a KOPR blocker may be useful for treatment of addictive disease.” In this image, KOPRs are stained in red; the blue-stained areas are nuclei of cells; and the green-stained regions are tyrosine hydroxylase, an enzyme involved in dopamine and norepinephrine synthesis, part of the brain’s reward and stress response system. SUMMER 2019 | TEMPLE HEALTH MAGAZINE |
45
Temple Health Magazine
Lewis Katz School of Medicine at Temple University Temple University Health System Office of Communications 3509 N. Broad Street Magazine Philadelphia, PA 19140
Temple Health
Temple Health Magazine
“During medical school, I developed deep connections to Temple’s neighbors and to the medical school community. Commitment to service isn’t just part of the curriculum at Temple; it’s a way of life.” BRENT HALSEY, MD 2019 Earned MA in Urban Bioethics along with the MD Liaison, Medical Alumni Association Board, 2019 President, Student Government Association, 2018-2019 Resident, Internal Medicine, Temple University Hospital, 2019-2022
K K K K
Help students become service-oriented physicians like Dr. Halsey, and make a gift today. giving.temple.edu/givetomed
NON-PROFIT ORGANIZATION U.S. POSTAGE
PAID PHILA, PA PERMIT 5140